Cryoglobulins, ANA, Scl-70, blood and fungal cultures were negative; complement levels were normal. His C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) had normalized.
He was admitted to our facility for possible APS and to rule out infective endocarditis in the setting of his recent dental work.
He had diminished dorsalis pedis and posterior tibial pulses, cyanotic changes in the distal tips of his toes, with blistering of toes one, two and three of his left foot. Capillary refill was extremely delayed in the affected toes, and he had ischemic changes with dark necrosis on the distal right hallux. The podiatric consultant opened the blister on the third toe, revealing clear serous fluid, which did not appear purulent. Intravenous (IV) vancomycin, IV ceftriaxone, heparin infusion, hydroxychloroquine and atorvastatin were started for limb-threatening distal ischemia in the context of his abnormal aPL profile. Blood cultures were negative, and a trans-esophageal echocardiogram was normal. The patient was discharged on warfarin, prednisone, hydroxychloroquine, nifedipine and atorvastatin.

FIGURES A–C: The patient’s left foot following first hospital discharge. FIGURE D: Digital ischemia, gangrene and cellulitis of the left foot one day prior to amputation. FIGURE E: The patient’s left foot three months post-amputation. (Click to enlarge.)
The patient was seen one week after discharge. He admitted to continued smoking, despite recommendations to quit. Prednisone tapering was started in view of the normal inflammatory markers. When seen by the podiatrist a week later, he was noted to have progressive gangrene of the left first and second toes, down to bone (see Figure 2 A–D), necessitating amputation of the first, second and third toes.
Surgical pathology revealed areas of gangrenous necrosis and did not mention any signs of vasculitis. The patient was discharged on long-term antibiotics for osteomyelitis. Over the next two months, prednisone was tapered off and the other medications continued. He continued to smoke. Despite this, his digital ischemia improved and the gangrene resolved. Three months following discharge he was doing well, with no signs of recurrent disease (see Figure 2E).
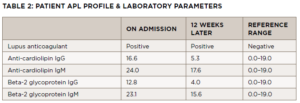
An antiphospholipid panel performed exactly 12 weeks following the initial panel revealed persistent positivity of the lupus anticoagulant, with anti-cardiolipin IgM and beta-2 glycoprotein IgM levels normalizing (see Table 2).
Discussion
Digital ischemia and gangrene requiring amputation are rare and potentially lethal complications of APS. Although not included in the classification criteria for APS, dermatologic manifestations of the disorder should be recognized and appropriately evaluated. The cutaneous findings of aPL are heterogeneous, with no singular pathognomonic feature. Livedo reticularis, cutaneous ulceration and necrosis, digital gangrene and subungual splinter hemorrhages are among the dermatologic findings described in a 1,000-patient aPL cohort study by Cervera et al.3