Tenderness to palpation of his cervical and thoracic spine was noted, and his range of motion in his neck and mid back was severely limited. His right knee was swollen and warm, and his range of motion was decreased due to pain. His left shoulder revealed warmth and swelling, and he had decreased range of motion on adduction and internal and external rotation. A full assessment of his strength was not possible, because pain prevented him from standing up.
Due to the severity and marked constitutional symptoms, he was admitted to the hospital for urgent evaluation. Laboratory analysis revealed elevated C-reactive protein (CRP) of 152.4 mg/L and an erythrocyte sedimentation rate (ESR) of 98 mm/hr. Screening for anti-nuclear antibodies (ANA), rheumatoid factor (RF), human leukocyte antigen B27 (HLA-B27), tuberculosis, human immunodeficiency virus antibodies, viral hepatitis, parvovirus serologies and chlamydial infection was all negative. His cerebrospinal fluid was evaluated for infection, and no evidence of bacterial, fungal or tuberculous meningitis was found.
X-rays of his left shoulder revealed mild periosteal elevation and hyperostosis of the proximal humerus and distal acromion, and the radiograph of his right knee revealed a subtle osteolytic, erosive lesion on the lateral side of the femur near the joint margin. Magnetic resonance imaging (MRI) of the cervical, thoracic and lumbar spine revealed multifocal, enhancing lesions consistent with marrow edema (see Figures 2A and 2B, below). The brain MRI did not reveal any intracranial lesions, but clearly revealed the cutaneous abscesses on his scalp (see Figure 2C).
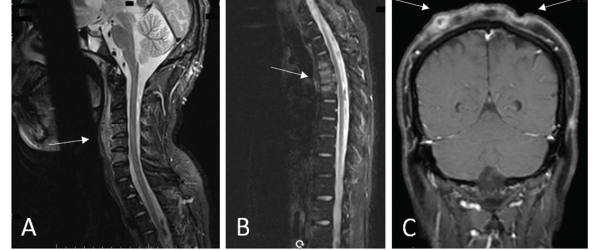
Figures 2a, b, c
(A) An MRI of the cervical spine revealed multilevel, anterior-predominant, marrow edema extending from C3–C7 with paravertebral edema anteriorly (see white arrow). (B) An MRI of the thoracic spine revealed marrow edema of T3–T5 with mild anterior, superior corner erosion of T5 (see white arrow). (C) An MRI of the brain revealed no intracranial lesions, but note the obvious cellulitis and abscess formation on the scalp (see white arrows).
A biopsy of the T4 vertebral body revealed no evidence of bacterial, acid-fast bacilli, fungal or mycobacterial infection. Surgical pathology of the T4 vertebra revealed only hypercellular marrow tissue without evidence of malignancy.
Presumptive diagnosis: undifferentiated spondyloarthropathy, given his axial and peripheral inflammatory disease. Initial therapy included prednisone and methotrexate.
Clinically, he showed some improvement and was discharged to follow-up care with dermatology and rheumatology clinics. Dermatology performed a biopsy of the scalp lesions that revealed histologic findings consistent with dissecting cellulitis of the scalp. He was also diagnosed with acne keloidalis nuchae.

