Discussion
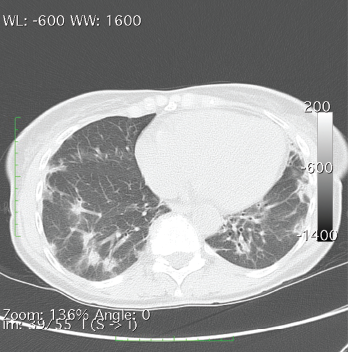
A CT of the chest without contrast showed multiple nodular and coalescing opacities involving the bilateral lungs diffusely, with more extensive involvement of the bibasilar regions.
Dermatomyositis encompasses a host of musculoskeletal and cutaneous symptoms, the latter of which are often heterogeneous in presentation. It is thought that differing serological responses, as reflected via various antibody markers, may represent differing immune responses, even unique phenotypes, with associated keratinocyte damage, which may explain the heterogeneity of presentation.4,5
MDA5, a receptor that binds with RNA and triggers a type I interferon response in infectious and inflammatory processes, was discovered in 2002 and has since become a point of interest in the study of autoimmune processes.6 Among patients with DM, certain features are strongly associated with anti-MDA5, including the absence of myositis and the presence of palmar papules, periungual, digital and elbow cutaneous ulcers, and rapidly progressive ILD, suggesting a unique phenotype that may pose its own treatment challenge.5
Initial treatment of DM often comprises anti-malarials, but there is no consensus on first-line therapy.3,7 Further, symptoms frequently require more aggressive treatment and a combination of multiple medications to achieve adequate control. Common additional agents include corticosteroids, calcineurin inhibitors (e.g., cyclosporine, tacrolimus), steroid-sparing immunosuppressants (e.g., methotrexate, azathioprine, cyclophosphamide, MMF) and intravenous immunoglobulin.8 Despite the use of these agents, symptoms often remain refractory.
Among patients with dermatomyositis, certain features are strongly associated with anti-MDA5, including the absence of myositis & the presence of palmar papules, periungual, digital & elbow cutaneous ulcers, & rapidly progressive ILD, suggesting a unique phenotype that may pose its own treatment challenge.
Recent advancements in biologics have introduced new treatment possibilities for DM. Therapies under investigation may be divided into those targeting B and T cells, and those targeting cytokines. Among these agents, rituximab, lenabasum, tofacitinib, apremilast, anakinra and tocilizumab have been promising in their effects on skin symptoms.3,9–13
In our patient with concurrent CADM and RA, agents that address both disease processes are of particular interest; the presence of ILD, common among CADM patients, adds further consideration to treatment choice. Rituximab, tofacitinib and tocilizumab, well studied in the treatment of RA, are of increasing interest in the treatment of CADM, given promising results in addressing skin symptoms.14
Regarding ILD, a suggested treatment approach is clinical evaluation and pulmonary function tests every three to six months, in addition to: 1) a combination of steroids and the choice of rituximab, cyclophosphamide or a calcineurin inhibitor for acute or severe pulmonary disease; or 2) a combination of steroids and the choice of MMF or azathioprine for chronic or milder ILD.15
These considerations ultimately led to our chosen treatment regimen of hydroxychloroquine, prednisone, MMF and rituximab.


