
Master1305 / shutterstock.com
We report on a 77-year-old patient who was diagnosed with giant cell arteritis (GCA) on histopathology of the submandibular gland and eventually went on to develop classic signs and symptoms of GCA. This observation highlights neck swelling as a rare initial presentation of GCA.
Case Presentation
A 77-year-old previously healthy man presented to his primary care physician with painless left-sided neck swelling of six months’ duration. Magnetic resonance imaging of the neck demonstrated diffuse homogenous enhancement of the left submandibular gland.
To exclude malignancy, he underwent excisional biopsy of the left submandibular gland, which showed active arteritis with multiple giant cells consistent with GCA, as well as chronic sialadenitis with fibrosis, gland dropout and patchy chronic inflammation, but no evidence of malignancy (see Figure 1). He was referred to a rheumatologist. He denied experiencing symptoms of GCA including headache, jaw claudication, scalp tenderness, fever, fatigue, weight loss, vision changes or polymyalgia rheumatica.
On physical examination, the patient was well appearing, and his temporal artery pulses were equal and without tenderness or nodularity. His erythrocyte sedimentation rate (ESR) was 6 mm/hr (normal: 0–20 mm/hr), his C-reactive protein (CRP) level was <1.0 mg/L, and his hemoglobin and alkaline phosphatase were also unremarkable. A vascular ultrasound of the temporal, subclavian and axillary arteries was normal.
Given the submandibular gland findings, prednisone was recommended for treatment of focal GCA; however, the patient declined treatment and instead remained under close clinical observation with his rheumatologist.
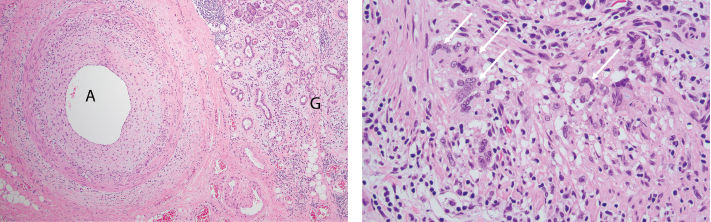
FigureS 1A (left) & 1B: Pathologic Findings of Submandibular Gland Resection
1A) A low-power photomicrograph demonstrates active giant cell arteritis with intimal proliferation and medial chronic inflammation consisting of lymphocytes, macrophages and occasional giant cells within a small artery (A). Chronic sialadenitis manifests as chronic inflammation, fibrosis and gland dropout in the glandular tissue (G). H&E stained section, 40x original magnification.
1B) A high-power photomicrograph demonstrates numerous giant cells (arrows) within the arterial wall. H&E stained section, 200x original magnification.
Eight months later, he developed pain in the right temple, as well as jaw pain with chewing. His ESR and CRP were elevated at 46 mm/hr and 41 mg/L, respectively. Vascular ultrasound was repeated and now showed hypoechoic circumferential wall thickening (i.e., halo sign) in the bilateral axillary arteries consistent with active arteritis in those vessels (see Figure 2). He was started on 40 mg of prednisone daily to treat GCA. His symptoms and inflammatory markers improved, and he was tapered off the prednisone within the subsequent two years without incident.
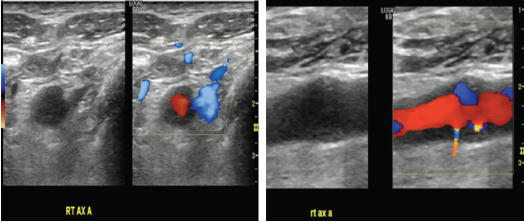
Figures 2a & 2B (from left): Vascular Ultrasound Images
Hypoechoic circumferential wall thickening of the right axillary artery is evident in transverse (A) and longitudinal (B) views.
Discussion
To our knowledge, submandibular swelling as an initial presentation of GCA has been reported only three times in the prior literature.1–3 In two of those cases, diagnosis of GCA was made on the basis of submandibular gland histopathology, as in our patient, and in the third, GCA was diagnosed on temporal artery biopsy. Clinical presentation in these reported cases varied with respect to presence of classic GCA features and inflammatory markers.
Ruiz-Masera et al. reported a case of a 75-year-old woman who presented with a painful right-sided submandibular mass; she had no systemic symptoms of GCA, and her ESR was normal.1 A resection of the submandibular gland mass showed GCA. Five months later, she developed symptoms of systemic GCA with headache, fever, fatigue, arthralgias and elevated ESR, and was treated with steroids.
Förderreuther et al. described a 72-year-old woman who presented with painful periorbital inflammation and submandibular swelling; she lacked other symptoms of GCA, and her ESR was normal.2 A submandibular gland biopsy revealed giant cell arteritis with extension of sclerosing inflammation into the surrounding soft tissue, and she was treated with prednisone and methotrexate.
Finally, Porter et al. reported the case of a 78-year-old woman who presented with several months of right-side submandibular swelling, as well as fever, scalp soreness and an elevated ESR.3 A temporal artery biopsy confirmed the diagnosis of GCA, and prednisone was commenced, leading to regression of the submandibular swelling, although the patient eventually passed away due to intracranial complications of GCA.
In addition to reporting a highly unusual presentation of GCA, our case demonstrates two additional clinical points.
First, branches of the external carotid artery—of which the superficial temporal artery is one—are targeted in GCA. Involvement of other branches of the external carotid system underlies many of the cranial manifestations of GCA (e.g., jaw claudication, facial swelling, dental pain, and pain and unusually overt necrosis of the tongue).4 In our patient, submandibular gland involvement almost surely resulted from arteritis of the gland’s primary blood supply from the submental and sublingual arteries, respectively branches of the facial and lingual arteries, both of which, in turn, are given off by the external carotid artery.
Second, the clinical presentation of GCA can occasionally appear to be clinically isolated, as has been described in the breast, female genitourinary tract and aorta.5–7
Our case underlines the importance of sustained vigilance for the emergence of explicit systemic arteritis, notwithstanding an apparently isolated presentation.
 Julia A. Ford, MD, is a recent graduate of the rheumatology fellowship at Brigham and Women’s Hospital, Boston, and is now a clinical assistant professor at the University of Michigan, Ann Arbor.
Julia A. Ford, MD, is a recent graduate of the rheumatology fellowship at Brigham and Women’s Hospital, Boston, and is now a clinical assistant professor at the University of Michigan, Ann Arbor.
 Robert Padera, MD, PhD, is an associate professor of pathology at Brigham and Women’s Hospital and Harvard Medical School.
Robert Padera, MD, PhD, is an associate professor of pathology at Brigham and Women’s Hospital and Harvard Medical School.
 Lindsey A. MacFarlane, MD, MPH, is an instructor in medicine at Harvard Medical School and a member of the rheumatology faculty at Brigham and Women’s Hospital.
Lindsey A. MacFarlane, MD, MPH, is an instructor in medicine at Harvard Medical School and a member of the rheumatology faculty at Brigham and Women’s Hospital.
Acknowledgment
The authors thank William Docken, MD, and Magda Abdou, RVT, for their assistance in preparing this article.
References
- Ruiz-Masera JJ, Alamillos-Granados FJ, Dean-Ferrer A, et al. Submandibular swelling as the first manifestation of giant cell arteritis. Report of a case. J Craniomaxillofac Surg. 1995 Apr;23(2):119–121.
- Förderreuther S, Ihrler, Küchle CCA. Giant cell arteritis presenting as a periorbital pain syndrome and a submandibular mass. Cephalalgia. 2003 May;23(4):314–317.
- Porter MJ. Temporal arteritis presenting as a submandibular swelling. J Laryngol Otol. 1990 Oct;104(10):819–820.
- Zaragoza JR, Vernon N, Ghaffari G. Tongue necrosis as an initial manifestation of giant cell arteritis: Case report and review of the literature. Case Rep Rheumatol. 2015;2015:901795.
- McKendry RJ, Guindi M, Hill DP. Giant cell arteritis (temporal arteritis) affecting the breast: Report of two cases and review of published reports. Ann Rheum Dis. 1990 Dec;49(12):1001–1004.
- Butendieck Jr RR, Abril A, Cortese C. Unusual presentation of giant cell arteritis in 2 patients: Uterine involvement. J Rheumatol. 2018 Aug;45(8):1201–1202.
- Talarico R, Boiardi L, Pipitone N, et al. Isolated aortitis versus giant cell arteritis: Are they really two sides of the same coin? Clin Exp Rheumatol. May-Jun 2014;32(3 Suppl 82):S55–S58.


