Psoriatic Arthritis Described
PsA is a complex rheumatologic disease that manifests in multiple individual patterns of musculoskeletal and skin involvement. Its hallmark features include inflammatory musculoskeletal disease in the presence of active or historical psoriasis skin inflammation, or a genetic predisposition to psoriasis through family history in a first- or second-degree relative. Psoriasis prevalence in the U.S. is 2%, and roughly one in three people with psoriasis develop PsA.1
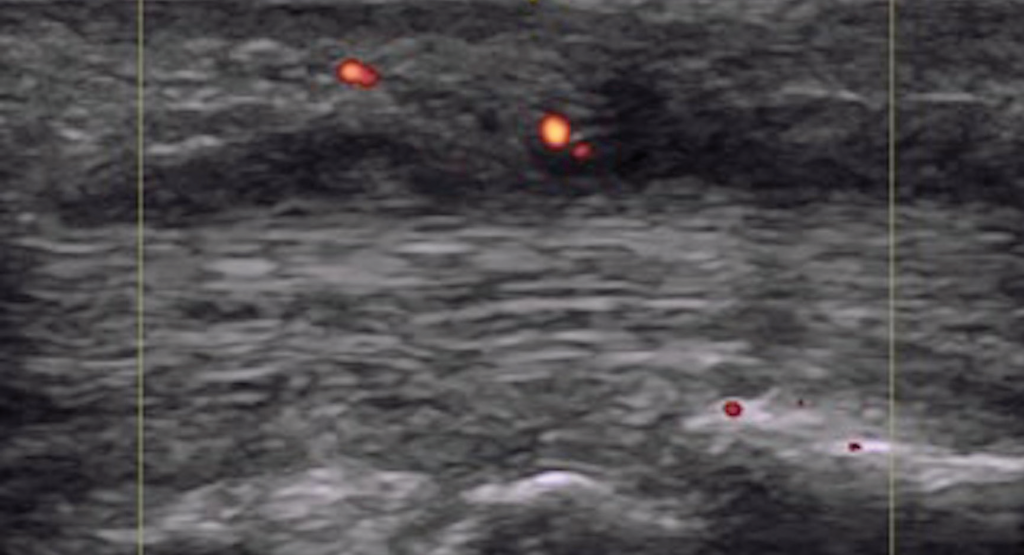
Figure 5. Dactylitis with flexor tenosynovitis and tendon Doppler enhancement.
A study from Toronto recently described the symptoms experienced by people with psoriasis prior to a PsA diagnosis: joint pain, fatigue and stiffness.2 Classification criteria for PsA are based on clinical evaluation and exclusion of rheumatoid arthritis (see Table 2). The presence of nail psoriasis and dactylitis increase specificity for a PsA classification.
Psoriatic Dactylitis & Enthesitis
Dactylitis and enthesitis are established, disease-specific manifestations in PsA. Each affect roughly half of the patients over their lifetime, and they are associated with increased disease burden and worse patient outcomes compared to patients who do not experience these manifestations. Pathophysiology of dactylitis and enthesitis are objects of intense study, as are their longitudinal quantification and measurement.
Dactylitis is defined as inflammation affecting all anatomical layers of a digit. Acute dactylitis is tender. Permanent damage has been demonstrated in digital joints affected by dactylitis, so it has a prognostic role as a sign of disease severity. In the CASPAR classification study, dactylitis increased the odds of PsA by 5.5–20 (historical dactylitis 5.5 and 95% CI 1.8–17; acute dactylitis 20 and 95% CI 5.9–67).
Enthesitis is defined as inflammation localized to the insertion sites of tendons and ligaments at the bony surface. The human body has more than 100 entheses; examples include the Achilles tendon insertion at the calcaneus, the annulus fibrosus insertions at the vertebral bodies, the sacroiliac joints and the flexor tendon insertions of the phalanges.
Enthesitis is a prominent feature of PsA and is included as part of the stem for the 2006 CASPAR criteria.3 Enthesitis leads to greater overall disease burden with poorer functional status, greater patient-reported pain and fatigue, and impairment of work and activities.4
Epidemiology
A diagnosis of dactylitis is based on clinical appearance and is best described as a sausage digit (see Figures 1 and 2). Dactylitis occurs in 40% of adult patients with established PsA.5 Examination of the feet is critical in diagnosing dactylitis because it can occur equally in fingers and toes. In the U.S. multicenter CORRONA PsA registry, prevalence of dactylitis in a cross-sectional PsA sample measured 15%.4 Dactylitis can occur in patients who are already taking PsA treatments, and when that happens, it is a sign of active or poorly controlled psoriatic disease.


