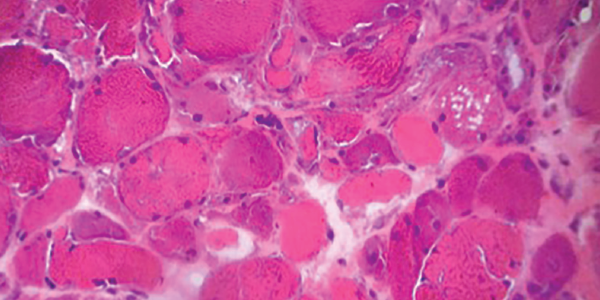
Figure 5. H&E staining of a muscle biopsy demonstrates myopathic changes, fiber necrosis and fiber atrophy, albeit a paucity of inflammatory cells.
MHC-I immunohistochemical staining showed patchy sarcolemmal up-regulation and an increased alkaline phosphatase staining pattern, consistent with an immune-mediated myopathic process. Electron microscopy of the muscle sample showed tubuloreticular inclusions (see Figure 6).
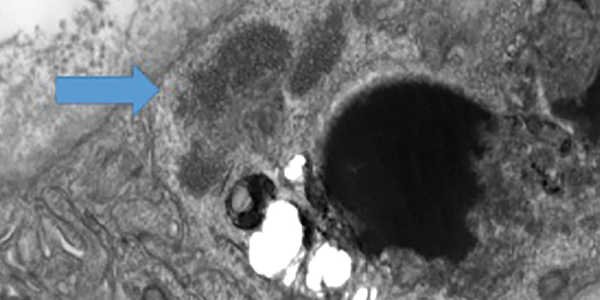
Figure 6 . Electron microscopy of a muscle biopsy shows tubuloreticular inclusions (blue arrow).
Our patient was diagnosed with dermatomyositis and began therapy with 1 mg/kg of oral prednisone daily on hospital day (HD) 2.
On HD 5, he started to experience intermittent, deep, throbbing inguinal pain on the left side. Examination of the area revealed no cutaneous abnormalities, palpable mass, tenderness to palpation or significant pain with passive range of motion.
On HD 7, his hemoglobin dropped to 6.9 g/dL, and his blood pressure acutely dropped to 74/36 mmHg. Upon review of his laboratory studies, his CK had risen from 793 U/L on HD 5 to 1,100 U/L on HD 6 and to 1,729 U/L on HD 7. Prothrombin time and prothrombin INR were within normal range. Partial thromboplastin time was minimally elevated.
An ultrasound of his left groin showed a 6.9×2.3×4.4 cm anechoic collection most suspicious for a hematoma. A CT scan of his abdomen and pelvis with and without contrast revealed multiple intramuscular hematomas in the left psoas, left abductor magnus/pectineus and left rectus femoris.
His blood pressure normalized with blood products and intravenous fluids. With ongoing sensation of dysphagia and concern for severe features of dermatomyositis, treatment began with intravenous immunoglobulin (IVIG) 10% 0.5 g/kg per day on HD 9 for four days.
Notably, he had 10 doses of prophylactic subcutaneous heparin from HD 2 to HD 6. The hematomas were managed conservatively, and he recovered from the acute episode with supportive care. He received systemic chemotherapy for adenocarcinoma of presumed lung origin, started a slow oral prednisone steroid taper from 1 mg/kg per day, and was discharged to a long-term rehabilitation facility.
As an outpatient, he did not tolerate aggressive treatments with intravenous chemotherapy, suffering from recurrent pulmonary infections that left him with an oxygen requirement and mostly bedbound. In view of this, he transitioned to a lower potency oral chemotherapeutic agent given his overall poor prognosis. Due to difficulty coordinating treatments and his ongoing health decline, he received no further IVIG. No additional hemorrhagic events were reported. Sadly, the patient died within a few months of discharge.


