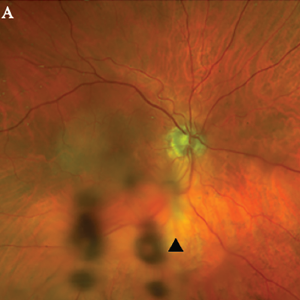
Figure 1A. Optos Fundus photo of the right eye with subtle area of retinal whitening in the macula with mild vitreous opacities inferiorly (arrowhead).
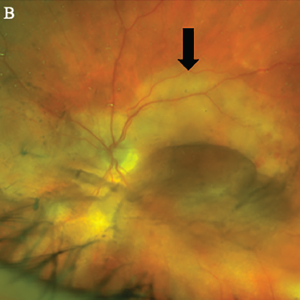
Figure 1B, Optos Fundus photo of the left eye with large placoid area of retinal whitening involving the macula (arrow), with retinal hemorrhages and vitreous opacity temporally.
He denied any eye pain, pain on eye movements, complete vision loss, new neurologic symptoms, fevers, chills, fatigue, weight loss or jaw claudication.
In the clinic, the initial fundoscopic exam appeared normal. Inflammatory markers were significantly elevated with a C-reactive protein (CRP) level of 35.8 mg/L and an erythrocyte sedimentation rate (ESR) of 130 mm/hour.
He was referred to the emergency department with a concern for giant cell arteritis.
On initial examination, patient was afebrile with stable hemodynamics. Bilateral temporal artery pulses were present and equal. There was no temporal artery nodularity or tenderness to palpation on either side.
Magnetic resonance imaging (MRI) of the brain showed chronic microvascular ischemic changes, but no changes in the orbit or optic nerve. He received pulse-dose steroids with 1,000 mg of intravenous (IV) methylprednisolone daily for three days for presumed GCA, and was continued on 60 mg of oral prednisone daily. A bilateral temporal artery biopsy was performed, but was unrevealing.
The patient said his right eye vision and right temple pain improved with steroids. Given the high clinical suspicion for GCA and the improvement in his symptoms, the decision was made to continue treatment with steroids.
The patient presented to the rheumatology clinic in follow-up a few weeks later. At the time of the visit, he reported a new-onset sharp pain and blurry vision in the left eye. He denied headaches at that time and had an unrevealing physical exam. Due to his new onset of visual symptoms despite being on high-dose steroids, as well as previously negative temporal artery biopsy results, GCA was presumed to be unlikely etiology and a steroid taper was initiated by the rheumatologist.
The patient was reevaluated by an ophthalmologist to address the new vision changes. Subsequent ophthalmologic exam showed bilateral placoid lesions involving the macula, characteristic for syphilitic placoid chorioretinitis (see Figures 1A&B and 2).
As a part of his broader workup, a test for Treponema pallidum was ordered. A plasma reagin (RPR) test was positive, with titers at 1:128. A fluorescent treponemal antibody absorption (FTA-Abs) test was also positive.
The patient was referred to an infectious disease specialist for further management. At the time of infectious disease visit, his sexual history was confirmed, and he reported a homosexual encounter with a new partner about three weeks prior to presentation. No protection was used at the time.
Further tests for infectious diseases were negative for HIV and hepatitis C. Based on his clinical presentation and high-risk sexual exposure, the diagnosis of ocular syphilis was made.
The patient had no other neurological complaints, so a decision to obtain lumbar puncture for cerebrospinal fluid (CSF) analysis was deferred. The patient completed a 14-day course of IV penicillin. He has been closely followed up by infectious disease and ophthalmology teams. His visual symptoms improved subjectively and objectively on follow-up with ophthalmology.


