Despite acetaminophen use during his seven-day hospitalization, the patient’s temperature waxed and waned, with a documented maximum temperature of 102.5ºF. He experienced continued fevers despite intravenous antibiotic treatment for the first 72 hours of hospitalization, thus his regimen was broadened to include daptomycin, meropenem and doxycycline.
The patient continued to have significant elevation of his ferritin levels, joint pain and fevers, suspicious for hemophagocytic lymphohistiocytosis (HLH)/macrophage activation syndrome (MAS). On hospital day 4, 1 g of intravenous methylprednisolone daily for three days was initiated, which led to reduced joint pain and decreased fevers.
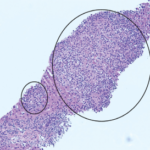
To further evaluate for HLH, a bone marrow biopsy was performed on hospital day 5, demonstrating hemophagocytosis, consistent with HLH/MAS. The bone marrow biopsy also revealed hypercellular bone marrow, trilineage hematopoiesis without abnormal B cells or blasts on flow cytometry, which reduced the likelihood of a bone marrow malignancy.
The soluble IL-2 alpha receptor level was elevated at 2,202 U/mL (normal: 858 U/mL).
Prior to discharge, the patient was transitioned from intravenous methylprednisolone to 60 mg of oral prednisone daily, with trimethoprim/sulfamethoxazole for prophylaxis against Pneumocystis.
While on a slow steroid taper, the patient developed steroid-induced psychosis, thus was tapered off steroids over the following two weeks. During this time, he continued to have joint pain; thus, 100 mg of subcutaneous anakinra daily was prescribed.
For six months following initiation of anakinra, the patient complained of diffuse pruritus and dry cough, which he attributed to the anakinra. The anakinra was discontinued, and the patient started canakinumab. He continued to have knee and shoulder pain; thus, 25 mg of subcutaneous methotrexate weekly was added, and his joint pain resolved.
One year following the onset of AOSD, the patient began to complain of dry eyes and dry mouth and was found to be anti-SSA antibody positive. Hydroxychloroquine was added to his regimen.
The patient is now stable and asymptomatic on canakinumab, methotrexate and hydroxychloroquine. He is able to live an active life with his wife and three young children.
Discussion
Adult-onset Still’s disease is a condition defined by a systemic inflammatory response whose pathogenesis remains unclear. The annual incidence of AOSD is 0.16 per 100,000 people.11 However, delays in diagnosis make it likely that the incidence is higher.1 There is apparently a bimodal distribution in the age of onset, with peaks between 15–25 years of age and 36–46 years of age. There also appears to be a higher occurrence among women, for unknown reasons.11,2