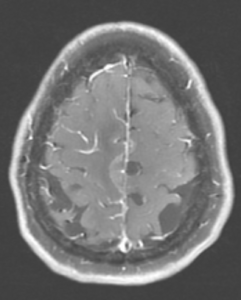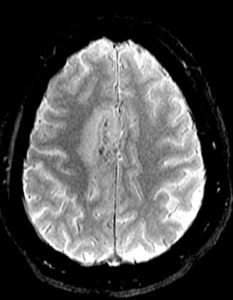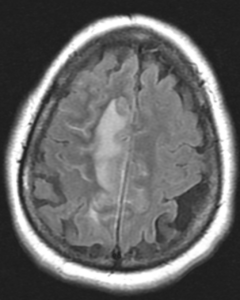
Figure 1A: T2/FLAIR sequence demonstrating right greater than left parasagittal frontal and parietal cortical T2/FLAIR hyperintensity and edema with involvement of the subcortical and deep white matter. There is also incomplete FLAIR suppression of the cerebrospinal fluid in the adjacent sulci, indicative of an inflammatory process. (Click to enlarge.)
Cerebral amyloid angiopathy (CAA) is a small-vessel disease of the central nervous system (CNS) characterized by amyloid-β deposition along the leptomeningeal and cortical vessels.1,2 Although CAA is a non-inflammatory process, an immunological response against the amyloid β peptides can develop in some patients, leading to an inflammatory, vasculitic CAA.2
Inflammatory CAA has a heterogeneous presentation sometimes mimicking CNS vasculitis, CNS infection and malignant conditions, posing a significant diagnostic challenge.3-6 The condition has two pathologically recognized subtypes: inflammatory-related CAA (CAAri), characterized by perivascular inflammatory infiltrates; and amyloid β-related angiitis (ABRA), characterized by more widespread vessel involvement with transmural, granulomatous infiltrates.7
Patients with CAAri respond to immunosuppressive treatment, so an early and accurate diagnosis is essential.5,8 Clinical and radiological criteria have been validated recently, but invasive diagnostic procedures, such as brain biopsy, remain the gold standard.9
Here, we present a case of inflammatory CAA, discussing its diverse clinical manifestations, diagnostic challenges in view of recently proposed clinical-radiologic criteria and its management.
Case Description
A 72-year-old woman, with a history of hypertension, hyperlipidemia and cutaneous porphyria, presented to a local hospital with a 10-day history of headache and recurrent falls. Upon initial encounter, the physical examination was remarkable for left-sided weakness in the arm (4/5) and leg (1/5), and gait instability.
Magnetic resonance imaging (MRI) of her brain revealed a right parasagittal T2/FLAIR, and cortical and subcortical white matter hyperintensity with gyral enhancement concerning for primary or metastatic malignant disease.
Cerebrospinal fluid examination revealed lymphocytic pleocytosis with elevated protein and immunoglobin G index, raising concern for an inflammatory process, such as multiple sclerosis. Due to diagnostic uncertainty, the patient was referred to our hospital for further investigation.
On arrival at our hospital, the physical examination demonstrated left-sided hemiparesis. Computed tomography (CT) scans of the chest, abdomen and pelvis did not reveal pathologic findings, with no signs of malignancy.