A repeat brain MRI showed a 2.3 cm x 0.9 cm enhancing lesion in the right parasagittal frontal lobe, with extensive leptomeningeal involvement, multiple foci of hemorrhage within the regions of enhancement, and associated vasogenic edema (see Figure 1). MRI spectroscopy showed necrotic tissue, with findings less consistent with glial neoplasm, lymphoma or demyelinating disease (see Figure 2).
Due to inconclusive findings, an open right frontal lobe biopsy was performed. Preliminary results were consistent with necrotizing granulomatous vasculitis (i.e., necrotizing vasculitis including vessels with fibrinoid necrosis in a background of marked inflammation with CD68+ giant cells). No indications of lymphoma, glial neoplasm or microorganisms were found.
Differential diagnoses at that time included primary angiitis of the CNS, isolated CNS sarcoidosis and systemic granulomatous vasculitis.
A review of systems was unremarkable. Inflammatory markers were notable for a mildly elevated C-reactive protein (CPR; 1.4 mg/L) but normal erythrocyte sedimentation rate (ESR; 26 mm/hr), and an extensive autoimmune evaluation was negative. A temporal artery ultrasound was performed, showing no evidence of temporal arteritis. A review of the CT images also did not reveal any signs of systemic vasculitis or sarcoidosis.
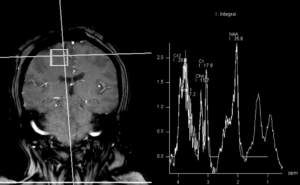
Figure 2: MRI spectroscopy demonstrated decreased NAA (N-acetylaspartate) peak without significant elevation of the choline peak. Findings are suggestive of a necrotic inflammatory process. Spectral features were inconsistent with glial neoplasm or other neoplastic etiologies, such as lymphoma or metastasis. (Click to enlarge.)
Given a low suspicion for infection, empiric treatment was started with pulse-dose glucocorticoids (1 g daily for three days), followed by 1 mg/kg/day of methylprednisolone. The patient exhibited rapid clinical response, with initial improvement in left upper arm strength within days of glucocorticoid initiation. The patient was discharged to a rehabilitation center and received six doses of cyclophosphamide as an outpatient, while remaining on low-dose prednisone (5 mg daily).
The final pathology report showed strong positive staining of the subarachnoid and parenchymal vessels with amyloid β, establishing the diagnosis of inflammatory cerebral amyloid angiopathy (CAA), specifically the cerebral amyloid β-related angiitis (ABRA) subtype (see Figure 3).
At a six-month follow-up in the rheumatology clinic, the patient demonstrated substantial clinical improvement, with complete resolution of her headaches, recovery of left upper extremity strength and improvement in left lower extremity weakness (4/5).
Discussion
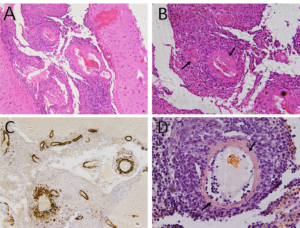 Figure 3A: Hematoxylin and eosin stain demonstrates small to medium-sized vessels that show necrotizing, fibrinoid necrosis representing a necrotizing vasculitis (100x).
Figure 3A: Hematoxylin and eosin stain demonstrates small to medium-sized vessels that show necrotizing, fibrinoid necrosis representing a necrotizing vasculitis (100x).


