A 53-year-old man was hospitalized for pericarditis, abdominal lymphadenopathy of unknown origin and non-bloody diarrhea. He was admitted for four days, and then he was discharged home without incident.
Two months after his initial presentation, he was readmitted for the evaluation of several new issues, including symmetric arthralgias, hypovolemia with associated electrolyte abnormalities and concurrent weight loss. On arrival at the emergency department, his mental status was altered, but it improved after intravenous fluids were started and returned to baseline within 24 hours.
The arthralgias had started six weeks prior to his new admission. The joint pain had started in his left wrist. It then spread to the knees, ankles, hips and shoulders. The pain did not worsen with activity and was not relieved by rest. The patient reported he had noticed progressive hand swelling. His pain had worsened to the point that walking was unbearable. He reported fever, loss of appetite, nausea and vomiting. He also reported having had one or two extremely watery, mucous-laden stools just prior to his emergency department visit.
On admission, the patient was noted to have numerous laboratory abnormalities: hyponatremia with a sodium level of 130 mEq/L (reference range [RR]: 136–145); hypokalemia with potassium at 3.0 mEq/L (RR: 3.5–5.1); a chloride level of 92 mEq/L (RR: 98–107); hypocalcemia with a level of 7.9 mg/dL (RR: 8.5–10.1); aspartate aminotransferase of 109 units/L (RR: 15–37); alanine aminotransferase of 84 units/L (RR: 12–78); elevated alkaline phosphatase of 158 units/L (RR: 45–117); C-reactive protein of 19 mg/dL (RR: 0–0.3); an erythrocyte sedimentation rate (ESR) of 95 mm/hr (RR: 0–20); thyroid-stimulating hormone of 6.46 µIU/mL (RR: 0.36–3.74); albumin of 1.3 gm/dL (RR: 3.4–5.0); prothrombin time of 16.6 seconds (RR: 9.0–12.5); international normalized ratio of 1.6 (RR: 0.8–1.2); a white blood cell count of 21,900/µL (RR: 4,000–11,000), with an increase in the number of immature leukocytes; hemoglobin of 8.0 g/dL (RR: 12.0–18.0); hematocrit of 24.9% (RR: 36.0–55); and a platelet count of 445,000 µL (RR: 125,000–400,000), with a left shift noted on admission. His corrected calcium was 9.9 mg/dL (RR: 8.5–10.1).
Given the patient’s diarrhea, he underwent a polymerase chain reaction (PCR) test for Clostridium difficile, which was negative. Blood cultures and stool cultures did not reveal an infectious etiology. A rheumatologist was then consulted for evaluation of his symmetric inflammatory polyarthralgias with concurrent lymphadenopathy.
The patient denied any history of blood clots, seizure or stroke. He had no history of leukopenia, thrombocytopenia or anemia. He had no known family history of systemic lupus erythematosus, gout, psoriasis or rheumatoid arthritis. He did complain, however, of having dry eyes, dry mouth and pharyngitis.
The physical exam of the patient revealed a pink-tinged, pruritic, circumferential rash encompassing his neck and chest. He had abdominal distension with mild hepatosplenomegaly, but without evidence of ascites. We noted symmetric polyarthritis, involving both wrists, distal interphalangeal joints, proximal interphalangeal joints, metacarpophalangeal joints and his elbows. Palpable synovitis of the shoulders, knees and ankles was also noted. Trochanteric and subacromial bursitis was present bilaterally.
Tests for anti-nuclear antibodies (ANA), rheumatoid factor, cyclic citrullinated peptide (CCP) antibodies, double-stranded DNA, anti-Smith antibodies and anti-RNP antibodies were negative. C3 and C4 levels were within the normal range. Syphilis serology, hepatitis serology and HIV tests were all negative. Anti-streptolysin screening was negative as well. Creatine kinase levels were within the normal range; his myoglobin was 63 ng/mL (RR: 10–92), and his uric acid was 2.2 mg/dL (RR: 2.6–7.2). His ferritin was elevated at 1,906.8 ng/mL (RR: 8–388).
A computed tomography (CT) scan of the abdomen and pelvis was obtained to evaluate his lymphadenopathy, abdominal pain and diarrhea. The CT scan showed upper abdominal retroperitoneal lymphadenopathy, which was nonspecific in appearance and did not demonstrate evidence of necrosis or adjacent inflammatory changes (see Figure 1, above).
A diagnosis of adult-onset Still’s disease was suspected due to his clinical presentation and fulfillment of the Yamaguchi and Fautrel’s classification criteria.1,2 All major and minor criteria, with the exception of a fever, were satisfied. He had demonstrated persistent arthralgias for more than two weeks and experienced a sore throat, transient erythematous rash, leukocytosis with a left shift, lymphadenopathy, hepatosplenomegaly, elevated aminotransferases, negative rheumatoid factor and negative ANA (see Tables 1 & 2).
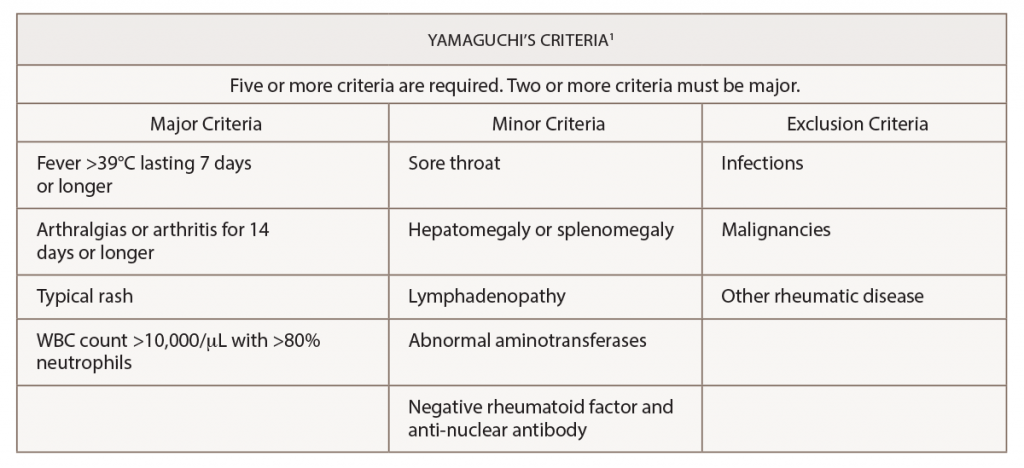
(click for larger image) Table 1: Yamaguchi’s Criteria for the Diagnosis of Adult-Onset Still’s Disease
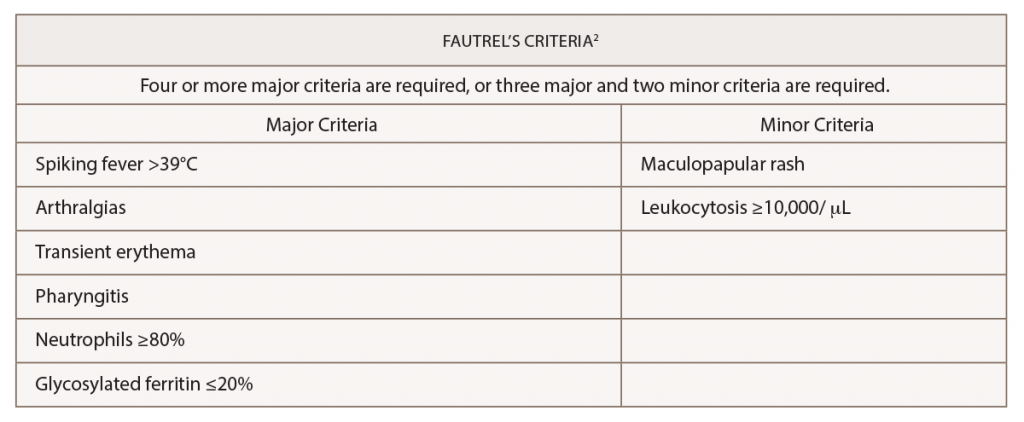
(click for larger image) Table 2: Fautrel’s Criteria for the Diagnosis of Adult-Onset Still’s Disease
The patient was started on 40 mg of methylprednisolone intravenously every eight hours.
Interventional radiology was consulted for biopsy of the retroperitoneal lymphadenopathy, but the biopsy proved to be technically difficult. On the advice of a hematologist/oncologist, an outpatient positron emission tomography (PET)/CT scan was arranged for further evaluation. During his hospital course, he developed bilateral deep venous thromboses, and he was started on 10 mg of apixaban twice daily for seven days and was then transitioned to 5 mg twice daily. His response to intravenous glucocorticoids was substantial, improving his synovitis, range of motion and pain. He was transitioned to 10 mg of oral prednisone daily and was discharged home.
Approximately two weeks after discharge, he returned to the hospital following a syncopal event. A magnetic resonance imaging (MRI) scan of his brain demonstrated multiple patchy areas of acute ischemia in the cerebellum consistent with an acute stroke. He reported compliance with the apixaban after hospital discharge; however, he had stopped taking the steroids, and the symmetric inflammatory arthritis had recurred.
Due to his persistent abdominal lymphadenopathy, bilateral deep venous thromboses, a guaiac-positive stool test and the recent stroke, which was thought to be thromboembolic despite anticoagulation, we were concerned about the possibility of a paraneoplastic hypercoagulable state. A gastroenterologist was consulted for endoscopic evaluation to aid the investigation into the abdominal lymphadenopathy (see Figure 2, above). Evaluation revealed a large, 4 cm polypoid, ulcerated, friable lesion in the distal esophagus. A biopsy of the lesion demonstrated an invasive, moderately differentiated adenocarcinoma. Of note, mutations in the Kirsten rat sarcoma viral oncogene homolog (KRAS) and TP53 genes, as well as PD-L1, were revealed.
The final diagnosis: a paraneoplastic syndrome caused by an esophageal adenocarcinoma, which mimicked adult-onset Still’s disease.
Discussion
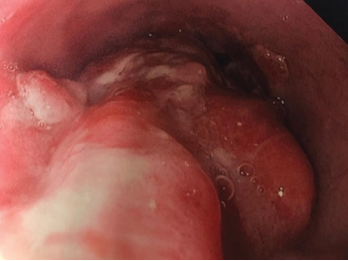
Figure 2. Endoscopy findings reveal distal esophageal adenocarcinoma.
Adult-onset Still’s disease is an inflammatory disorder characterized by leukocytosis, elevated ferritin levels, intermittent fevers and transient rashes.1 The Yamaguchi criteria are commonly used to assist with diagnosis. Fever for longer than one week, arthralgias or arthritis for two weeks, evanescent skin eruption and leukocytosis (10,000/µL or greater with 80% or greater neutrophils) are the major criteria used for the diagnosis of adult-onset Still’s disease. Absence of rheumatoid factor and anti-nuclear antibodies, and the presence of lymphadenopathy, pharyngitis, hepatomegaly, splenomegaly and abnormal aminotransferases are minor criteria that can be used to fulfill a diagnosis of adult-onset Still’s disease.
The exclusion of other illnesses is necessary to establish a diagnosis of adult-onset Still’s disease.1 Cancer and infection can mimic its clinical manifestations.3
Mutations in the KRAS gene have been reported, with lower overall survival in patients with colorectal cancer.4 KRAS mutations have also been associated with treatment resistance.5 The significance of the PD-L1 mutation is less clear. Hsieh et al. showed that overexpression of PD-L1 in patients with esophageal squamous cell carcinoma had a better overall survival after esophagectomy.6 The TP-53 mutation is associated esophageal and gastric carcinogenesis.7
Back to our patient: After initial treatment with intravenous methylprednisolone, our patient was treated with a gradual steroid taper; three weeks later his ferritin had decreased to 551 ng/mL (RR: 8–388), and his ESR had decreased to 51 mm/hr (RR: 0–20).
Interestingly, there is a case report of a patient with adult-onset Still’s disease who was diagnosed with an esophageal cancer nine months after the onset of Still’s disease.8 Shibuya et al. presented the case of a 77-year-old man who presented with adult-onset Still’s disease and had been placed on tapering doses of prednisolone. During the steroid taper, the patient developed recurrent fever, arthritis and rash. On re-evaluation, the patient was found to have esophageal cancer.8 This case highlighted that esophageal cancer may mimic adult-onset Still’s disease.
Our own case bears some similarities to this presentation. Our patient’s esophageal cancer was discovered shortly after he presented with adult-onset Still’s disease. Likewise, his rash and arthralgias worsened with lower steroid doses. In this regard, our patient presented in a fashion more typical of a paraneoplastic syndrome.
In 2015, Sun et al. described cases of malignancy associated with atypical presentations of adult-onset Still’s disease.9 Thirty-one case reports described patients who satisfied the Yamaguchi criteria (for a total of 31 patients), and adult-onset Still’s disease-like symptoms were reported in patients with multiple forms of malignancy. A diagnosis of a malignancy was established after a diagnosis of adult-onset Still’s disease in 13 of the 31 cases.
The condition most strongly associated with adult-onset Still’s disease-like symptoms was lymphoma (eight of the 31 patients).9,10 Breast cancer had the second strongest association (six of the 31 patients).9 Papillary subtypes of thyroid cancer were reported as well.9,11 With regard to the gastrointestinal tract, one malignancy of the esophagus and one malignancy involving the rectum were documented.9
The single case of esophageal cancer noted in this review was the patient presentation documented by Shibuya et al. in 2003.8 One patient was diagnosed with cholangiocarcinoma.9,12 The cutaneous findings associated with the adult-onset Still’s disease presentations were consistent with evanescent rashes in all but two of the 31 cases.9
According to Sun et al., the first reports of adult-onset Still’s disease-like symptoms in the setting of malignancy were described in 1988.9,13 The first patient was diagnosed with myeloproliferative syndrome, but had initially presented with fever, arthritis, leukocytosis and a transient rash. The second patient also initially presented with fever, arthritis and a temporary rash, but was later discovered to be harboring a laryngeal carcinoma.13
Charda et al. performed extensive chart reviews of patients aged 18 and older who were diagnosed with adult-onset Still’s disease or an adult-onset Still’s disease-type syndrome.14 Nine patients with adult-onset Still’s disease were identified and followed for 25 months after initial diagnosis. One developed Hodgkin’s lymphoma, and another had acute myelogenous leukemia with concurrent non-squamous cell lung carcinoma. This study suggested a relationship between adult-onset Still’s disease and malignancy needs to be explored and further supports the hypothesis that our patient’s initial presentation may have had a correlation with malignancy.
Conclusion
Our case highlights a rare presentation of a paraneoplastic syndrome presenting as adult-onset Still’s disease. The patient met Yamaguchi criteria for a diagnosis of adult-onset Still’s disease, but a diagnosis of esophageal cancer was made within weeks. This demonstrates the need for aggressive exclusion of underlying malignancy in cases of suspected adult-onset Still’s disease.
Theodore Korty, DO, is a first-year rheumatology fellow at Regional Medical Center Bayonet Point, Hudson, Fla.
Ken Baxa, DO, is a first-year rheumatology fellow at Regional Medical Center Bayonet Point, Hudson, Fla.
Kiren Sahni, DO, is a first-year rheumatology fellow at Regional Medical Center Bayonet Point, Hudson, Fla.
Adam Grunbaum, DO, is the rheumatology program director at Regional Medical Center Bayonet Point, Hudson, Fla.
Maria Soto-Aguilar, MD, is the rheumatology program core faculty at Regional Medical Center Bayonet Point, Hudson, Fla.
References
- Yamaguchi M, Ohta A, Tsunematsu T, et al. Preliminary criteria for classification of adult Still’s disease. J Rheumatol. 1992 Mar;19(3):424–430.
- Fautrel B, Zing E, Golmard JL, et al. Proposal for a new set of classification criteria for adult-onset still disease. Medicine (Baltimore). 2002 May;81(3):194–200.
- Bagnari V, Colina M, Ciancio G, et al. Adult-onset Still’s disease. Rheumatol Int. 2010 May;30(7):855–862.
- Lièvre A, Bachet JB, Le Corre D, et al. KRAS mutation status is predictive of response to cetuximab therapy in colorectal cancer. Cancer Res. 2006 Apr 15;66(8):3992–3995.
- Blanchard P, Quero L, Pacault V, et al. Prognostic significance of anti-p53 and anti-KRAS circulating antibodies in esophageal cancer patients treated with chemoradiotherapy. BMC Cancer. 2012 Mar 26;12:119.
- Hsieh CC, Hsu HS, Li AY, Chen YJ. Clinical relevance of PD-L1 and PD-L2 overexpression in patients with esophageal squamous cell carcinoma. J Thorac Dis. 2018 Jul;10(7):4433–4444.
- Bellini MF, Cadamuro AC, Succi M, et al. Alterations of the TP53 gene in gastric and esophageal carcinogenesis. J Biomed Biotechnol. 2012;2012:891961.
- Shibuya Y, Matuo K, Kawada T, et al. [Adult onset Still’s disease associated esophageal cancer: A case report.] [Article in Japanese] Ryumachi. 2003 Jun;43(3):577–582.
- Sun NZ, Brezinski EA, Berliner J, et al. Updates in adult-onset Still disease: Atypical cutaneous manifestations and associations with delayed malignancy. J Am Acad Dermatol. 2015 Aug;73(2):294–303.
- Rogues AM, Vidal E, Boudinet F, et al. Breast cancer with systemic manifestations mimicking Still’s disease. J Rheumatol. 1993 Oct:20(10):1786–1787.
- Ahn JK, Oh JM, Lee J, et al. Adult onset Still’s disease diagnosed concomitantly with occult papillary thyroid cancer: Paraneoplastic manifestation or coincidence? Clin Rheumatol. 2010 Feb;29(2):221–224.
- Raza A, Houk L, Yousaf W, et al. Unusual para-neoplastic manifestation of cholangiocarcinoma. J Gastrointest Cancer. 2013 Jun;44(2):228–230.
- Cabane J, Lebas J, Wattiaux MJ, Imbert JC. [Pseudo-Still disease and neoplasm. 2 cases]. [Article in French] Rev Med Interne. 1988 Jan–Feb;9(1):81–84.
- Chavda R, Bussey MR, Tehrani R, Ostrowski RA. The prevalence of malignancy in adult-onset Still’s disease [abstract]. Arthritis Rheum. 2014 Oct;66(Suppl 10):S545.


