Ezume Images / shutterstock.com
In certain ethnic populations and geographic locations, being a genetic carrier of sickle cell trait is common. Despite its prevalence, a recent report studied 100 mothers who were informed their newborn child had tested positive for sickle cell trait, and of these mothers less than half were aware of their carrier status prior to conception.1
Case Report
In 2017, a 65-year-old Black man was first seen for one week’s duration of pain in both knees and nodules on both of his forearms that he’d had for the past year. On the basis of a physical examination revealing polyarthritis of multiple joints, nodules and joint deformities, the patient was diagnosed with rheumatoid arthritis. This diagnosis was confirmed by lab results positive for rheumatoid factor and anti-cyclic citrullinated peptide antibody.
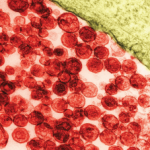
The patient had a right olecranon bursa, which the physician aspirated, and under microscopic analysis, the joint fluid revealed some rare white blood cells and rare red blood cells with occasional sickle cells. Hemoglobin electrophoresis confirmed that the patient had sickle cell trait.
The patient had no prior knowledge of his sickle cell carrier status, which is uncommon for a patient in his 60s. The diagnosis of sickle cell trait was an incidental finding based on the synovial analysis from his olecranon bursa. The presence of the patient’s olecranon bursitis in this case is suspected to be post-traumatic or related to his rheumatoid arthritis, not related to his sickle cell trait.
An Uncommon Incidental Finding
It is uncommon to diagnose sickle cell trait as an incidental finding in an unsuspected patient on the basis of joint fluid, although six cases have been reported. Five of the cases currently in the literature all presented with hemarthrosis. Glickstein et al. reported on the diagnosis of three patients who all presented with frank hemarthrosis.2 Casey et al. discussed another patient who presented with hemarthrosis and sickle cell trait.3
In a separate report, two patients were diagnosed as heterozygous for the sickle cell gene mutation via fluid analysis; one presented with hemarthrosis and the other without. The patient without hemarthrosis presented with tophaceous gout.4 It is unclear if the sickle cells caused the joint effusion in these cases, but in all six it was suspected to be an incidental finding.
In Sum
Our patient had a typical non-inflammatory olecranon bursitis with no hemarthrosis, and sickle cells were discovered incidentally. This appears to occur rarely based on the literature, but may be more common than we realize.
This case emphasizes the importance of a thorough synovial analysis. The diagnosis of sickle cell trait is clinically relevant because the patient may relay this genetic information to their relatives, particularly those of childbearing age.
 Mia Robb Stahler, DO, is a recent graduate of the Philadelphia College of Osteopathic Medicine. She became interested in med-icine through her own battle with rheuma-toid arthritis (RA), which she has had since she was a teenager. She attributes her ability to pursue a medical career to advances in RA treatment options.
Mia Robb Stahler, DO, is a recent graduate of the Philadelphia College of Osteopathic Medicine. She became interested in med-icine through her own battle with rheuma-toid arthritis (RA), which she has had since she was a teenager. She attributes her ability to pursue a medical career to advances in RA treatment options.
 Michael Rosen, MD, has been practicing rheumatology in Chester County, Pa., for 35 years. He completed his rheumatology fellowship at the University of Pennsylvania, Philadelphia. He has a private practice located outside of Philadelphia, affiliated with both Brandywine and Chester County Hospitals.
Michael Rosen, MD, has been practicing rheumatology in Chester County, Pa., for 35 years. He completed his rheumatology fellowship at the University of Pennsylvania, Philadelphia. He has a private practice located outside of Philadelphia, affiliated with both Brandywine and Chester County Hospitals.
References
- Vichinsky EP. Sickle cell trait. UpToDate.com. Viewed 15 July 2019.
- Glickstein SL, Melton 3rd JW. Sickled cells in synovial fluid: Clue to unsuspected hemoglobinopathy. South Med J. 1989 Jun;82(6):769–771.
- Casey DF, Cathcart ES. Hemarthrosis and sickle cell trait. Arthritis Rheum. Nov–Dec 1970;13(6):882–884.
- Hasselbacher P. Sickled erythrocytes in synovial fluids. Arthritis Rheum. 1980 Jan;23(1):127–128.