Granulomatosis with polyangiitis (GPA) is a small vessel vasculitis associated with anti-neutrophil cytoplasmic antibodies (C-ANCA), specifically proteinase 3 (PR3) ANCA. GPA classically presents with multi-organ involvement. The first description of GPA defined a triad of features: 1) systemic necrotizing angiitis, 2) necrotizing inflammation of the respiratory tract and 3) necrotizing glomerulonephritis.1
Few cases of digital limb ischemia have been reported in patients with GPA.2-5 Based on a literature review, digital limb ischemia in patients with GPA has an estimated prevalence of <1%.2
We present a case of GPA in which the primary complaint was digital limb ischemia.
Case
A 71-year-old woman, with a past medical history significant for migraines but no smoking history, presented initially with violaceous discoloration of her thumb and first two fingers on her right hand and fingers 2–5 on her left hand (see Figures 1). She reported that she’d been having pain, which was exacerbated with movement, for the previous week.
She underwent evaluation for digital limb ischemia, which was presumed secondary to vessel thrombosis. She was treated with a heparin, antiplatelet agent and hydroxyurea; however, this did not improve her ischemia. The patient then underwent thrombolysis of both arms, but her digital ischemia continued to progress.
A bone marrow biopsy, computed tomography angiography (CTA) of her chest and her renal function were all normal. Her rheumatoid factor and sedimentation rate were elevated, and she was positive for C-ANCA. The patient was then transferred to our facility for a rheumatology evaluation.

FIGURE 1B: Violaceous discoloration is present on the thumb and first two fingers of the right hand (i.e., digits 1–3) and four fingers on the left hand (i.e., digits 2–4). (Click to enlarge.)
Upon further evaluation, the patient reported that she’d had a sinus infection one month before presenting to the hospital. Additionally, she had developed new onset hemoptysis and hematuria the day before, along with left foot drop consistent with mononeuritis multiplex. With this additional information, the most likely differential diagnoses included cryoglobulinemic vasculitis, granulomatosis with polyangiitis, Raynaud’s syndrome, thromboangiitis obliterans and rheumatoid arthritis.
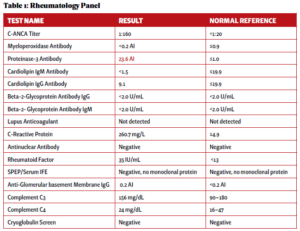
At this time, additional rheumatologic serologies were obtained, including myeloperoxidase (MPO), PR3, beta2-glycoprotein panel, complement levels, SPEP, ANA, glomerular basement membrane IgG, protein electrophoresis (see Table 1).
Laboratory results showed an elevated C-ANCA and PR3 and a protein normalized to creatinine ratio of 1,143 mg/g. Chest X-ray results showed increased airspace changes in both lungs, extending into the lower lobes. The rest of her serological work up was unremarkable.
In light of the positive ANCA serologies with pulmonary and renal manifestations, a diagnosis of granulomatosis with polyangiitis with digital limb ischemia was confirmed.
Plasmapheresis and pulse-dose methylprednisolone were initiated for five concurrent days. With plasmapheresis, her digital ischemia stabilized without further progression. After completion of this therapy, the patient was started on a combination of prednisone and rituximab, with improvement in symptoms over the treatment period (see Figure 2).
Upon discharge she was referred to hand surgery, hyperbaric oxygen therapy and acute rehabilitation. She underwent amputation after four months.

FIGURE 2: Progression of digital limb ischemia over two-week hospital course. Gangrenous progression occurred in digits 1–4 on the right hand and digits 2–5 on the left hand. (Click to enlarge.)
Discussion
Digital limb ischemia and gangrene are rare clinical manifestations of GPA.2-5
Lau et al. conducted a literature review and found 16 other case reports of GPA associated with digital limb ischemia.2 Since that case report publication in 2017, at least two other cases have been reported.3,4 According to previous studies, most cases of digital ischemia associated with GPA have presented with mainly upper extremity involvement, as seen in our patient.2
The most reported presenting signs and symptoms of GPA usually involve the ear, nose and throat (~73%), lungs (~45%), kidney (~18%) and eyes (~15%).6 Onset of common manifestations of GPA, such as hematuria and hemoptysis, did not present for at least one week into our patient’s hospital course. However, our patient did have an episode of sinusitis one month prior to onset of digital limb ischemia, consistent with GPA.
Digital ischemia and gangrene are more commonly associated with thromboangiitis obliterans, a medium vessel vasculitis.7 The pathophysiology of ischemia in vasculitis has been hypothesized to originate from the destruction of these vessels from active inflammation; however, arterial thrombi on biopsies have also been reported.2
Because digital limb ischemia is a rare presentation of small vessel vasculitis, the pathophysiology is not well studied; however, it has been presumed to be similar to the proposed pathophysiology of medium vessel vasculitis.2
Other case reports with digital limb ischemia associated with GPA have also reported mononeuropathy, as seen in our patient.3,8 This is a common clinical finding in vasculitis, resulting from ischemia of a focal nerve trunk.9 This finding further supported the diagnosis of GPA.
Patients with digital limb ischemia as the presenting symptom of GPA may have delayed diagnosis and treatment. With the rapid progression to multiple-organ involvement, early diagnosis and treatment are imperative in this patient population. Moreover, reported mortality rates of GPA are highest in the first six months of disease, and without correct and prompt treatment, digital limb ischemia can lead to severe disability.10
In Sum
We describe a 71-year-old woman who presented with digital limb ischemia as the primary complaint for GPA. Digital limb ischemia and gangrene are much more commonly found with a medium vessel vasculitis and have rarely been associated with GPA, with an estimated incidence of <1%. With the mortality rates of GPA being highest in the first six months of diagnosis, patients must be diagnosed and treated promptly. Thus, it is important to bring awareness to digital limb ischemia and gangrene as an associated, but rare, presenting cutaneous symptom of GPA.
Adina Greene, BA, is a third-year medical student at the University of Arizona College of Medicine, Phoenix, and a dermatology research fellow at Mayo Clinic Arizona.
Sabrina Dahak, MD, is a preliminary internal medicine intern at the University of Arizona College of Medicine, Phoenix, and will start her dermatology residency in July 2024 at Washington University in St Louis – Division of Dermatology.
Wesley A. Robertson, MD, graduated medical school from the University of Arizona College of Medicine, Tucson. He received his masters in public health and public policy from the University of Wisconsin. A current third-year resident at the University of Arizona College of Medicine, Phoenix, he is a future gastroenterologist.
Denege Ward-Wright, MD, graduated from Wayne State University School of Medicine, Detroit. She is board certified in internal medicine and a former assistant clinical professor at the University of Michigan, where she practiced primary care and hospital medicine. She is currently the associate clinical professor of internal medicine and associate chair of justice equity diversity and inclusion in the Department of Medicine at the University of Arizona College of Medicine, Phoenix.
Kristen Young, DO, MEd, is a clinical assistant professor of medicine and rheumatologist at the University of Arizona College of Medicine, Phoenix, and Banner-University Medical Center, Phoenix. Her research interests include medical education, interstitial lung diseases, access to care and patient-related outcomes in rheumatology.
References
- Godman GC, Churg J. Wegener’s granulomatosis: Pathology and review of the literature. AMA Arch Pathol. 1954 Dec;58(6):533–553.
- Lau RA, Bains R, Suraweera D, et al. A rare case of digital ischemia and gangrene in ANCA-associated vasculitis with review of the literature. Case Rep Rheumatol. 2017;2017:2421760.
- Hines A, Bello V, Iftikhar A, Zein H. Rare presentation of granulomatosis with polyangiitis. BMJ Case Rep. 2019 Feb 22;12(2):e227218.
- Pokharel S, Singh S, Shaukat MS. An unusual presentation of granulomatosis with polyangiitis (GPA). Am J Case Rep. 2018 Sep 7;19:1071–1073.
- Lim SY, Lim JH, Horn C. Upper-extremity digital ischemia in granulomatosis with polyangiitis. J Clin Rheumatol. 2014 Apr;20(3):155–159.
- DeRemee RA, McDonald TJ, Harrison EG Jr., Coles DT. Wegener’s granulomatosis: Anatomic correlates, a proposed classification. Mayo Clin Proc. 1976;51(12):777–781.
- Young C, Beynon H, Haskard D. Buerger’s disease (thromboangiitis obliterans): A reversible cause of upper limb digital infarcts. Rheumatology (Oxford). 2000 Apr;39(4):442–443.
- Modi M, Vats AK, Prabhakar S, et al. Acroosteolysis and mononeuritis multiplex as a presenting symptom of systemic angiitis of Wegener’s type. Indian J Med Sci. 2007 Apr;61(4):212–215.
- Koike H, Nishi R, Ohyama K, et al. ANCA-associated vasculitic neuropathies: A review. Neurol Ther. 2022 Mar;11(1):21–38. 10. Lin CY, Chen HA, Chang TW, et al. Time-dependent risk of mortality and endstage kidney disease among patients with granulomatosis with polyangiitis. Front Med (Lausanne). 2022 Aug 10;9:817204.