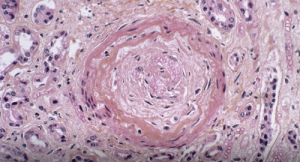
Light micrograph of a vascular lesion (center) caused by systemic sclerosis.
CNRI / Science Source
Systemic sclerosis (SSc) is a multi-system connective tissue disease in which skin and internal organ fibrosis are associated with an obliterative micro-vasculopathy and a degree of inflammation.1 Patients often report it takes one to three years from the appearance of the first signs and symptoms before they receive a diagnosis. The signs and symptoms of systemic sclerosis can be mistaken for any number of diseases, depending on the predominant symptom at the time of examination.3 Early detection provides the opportunity to manage the disease process before damage and fibrosis lead to organ failure and poor outcomes.4
A salt-and-pepper appearance of the skin is just one of many changes observed in the skin of patients with systemic sclerosis.5 It is one of the earliest cutaneous findings in systemic sclerosis.6 Occasionally, it may be the sole cutaneous manifestation.5
Below, we present a case of systemic sclerosis diagnosed five years from the first presentation, which was pseudo-vitiligo, i.e., salt-and-pepper skin pigmentation.
The Case
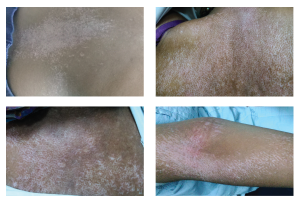
Figures 1, 2, 3 & 4
These photos show salt-and-pepper pigmentation over the patient’s upper back, trunk and upper extremity.
A 30-year-old female patient from Egypt presented to the rheumatology department with chief complaints of pain and swelling of both hands, and thickening and hardening of the skin over her extremities for the past two months. The patient had first become symptomatic in 2013, when her symptoms started as painless skin pigmentation over her neck, back and shoulder, which were diagnosed as vitiligo. At that time, she received systemic psoralen and ultraviolet A therapy for six months with a moderate response.
In April 2015, she had a history of heartburn and regurgitation, which she treated with antacids. In the winter of 2016, she developed Raynaud’s in her fingertips, which usually resolved after she warmed her hands.
Her past medical and family history was otherwise unremarkable. Her physical examination was notable for salt-and-pepper pigmentation over her back, chest and arms (Figures 1–4, below), and skin tightening over her fingers, hand and forearm. Her right wrist and all metacarpophalangeal joints were swollen and tender with normal range of motion. There was no associated digital pallor or cyanosis.
A 5 mm punch skin biopsy of the patient’s forearm was sent for histopathological examination, which demonstrated epidermal atrophy and perivascular lymphocytic and plasma cell infiltrates in the superficial and deep dermis (see Figure 5, p. 20). Her routine laboratory tests were unremarkable. Her anti-Scl-70 antibodies, anti-centromere antibodies, antinuclear antibody, thyroid function tests, rheumatoid factor, chest X-ray, pulmonary function testing, electrocardiogram and echocardiogram were normal. The clinical and histopathologic findings were consistent with a diagnosis of systemic sclerosis in our patient.
We treated the patient with oral prednisone, non-steroidal anti-inflammatory drugs, phosphodiesterase type 5 inhibitor, mycophenolate mofetil, prokinetics and a proton pump inhibitor. The patient symptomatically improved with regard to arthritis and gastrointestinal symptoms. We continue to see her in our outpatient clinic.
A salt-and-pepper appearance of the skin is … one of the earliest cutaneous findings in systemic sclerosis.
Discussion
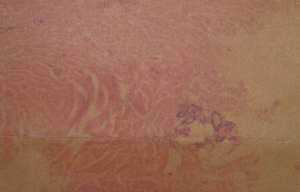
Figure 5. A skin biopsy revealed superficial and deep dermal perivascular lymphocytic infiltrate and focally increased dermal collageny.
Systemic sclerosis is a heterogeneous disorder characterized by dysfunction of the endothelium, dysregulation of fibroblasts (resulting in excessive production of collagen) and immune system abnormalities.7 Although the cause of SSc remains unknown, genetic and environmental factors are believed to contribute to host susceptibility.8 SSc is divided into diffuse cutaneous and limited cutaneous syndromes, depending on the extent of skin thickening. These classically manifest as Raynaud’s phenomenon, sclerodactyly, esophageal dysmotility and a range of organ-specific complications.1 Systemic involvement may occur in the form of pulmonary vasculopathy, interstitial fibrosis, cardiomyopathy, arrhythmia, conduction abnormality, acute renal crisis, etc.2
A salt-and-pepper appearance features patchy hypopigmentation and hyperpigmentation of the skin manifesting as vitiligo-like depigmentation with perifollicular pigmentary retention.5 Vitiligo and the depigmented lesions in SSc share many features. Clinically, both are characterized by chalk-white macules with well-defined borders. Both cellular and humoral immune factors, in combination with external factors such as trauma or inflammation, may trigger the destruction of melanocytes.6
In 2009, Adelowo et al. found that salt-and-pepper skin emerged as the most common presentation among 14 Nigerian SSc patients.10 In 2006, Sharma et al., in a study of 100 SSc patients performed at the All India Institute of Medical Sciences in New Delhi, found that 51% of SSc patients had a salt-and-pepper skin appearance.11
A salt-and-pepper skin appearance is just one of many changes observed in the skin of patients with systemic sclerosis, but we think paying attention to this sign may help early diagnosis of systemic sclerosis. And again, delayed diagnosis may be associated with complications, such as pulmonary fibrosis or hypertension, myocarditis, pericardial effusion, arthritis or renal involvement.
Wesam Gouda, MBBCh, MSc, is an assistant lecturer of rheumatology at Aswan University, Egypt.
Abdelhafeez Moshrif, MBBCh, MSc, MD, is a lecturer of rheumatology at Al-Azhar University, Assiut, Egypt.
Fatma H. El Nouby, MBBCh, MSc, MD, is a lecturer of rheumatology in the rheumatology department at Aswan University, Egypt.
Amal Fehr, MBBCh, MSc, MD, is a lecturer of rheumatology in the rheumatology department at Helwan University, Egypt.
References
- Allcock RJ, Forrest I, Corris PA, et al. A study of the prevalence of systemic sclerosis in northeast England. Rheumatology. 2004 May;43(5):596–602.
- Rai VM, Balachandran C. Pseudovitiligo in systemic sclerosis. Dermatol Online J. 2005 Dec 1;11(3):41.
- Mays MD. (1999) The Scleroderma Book: A Guide for Patients and Families. New York: Oxford University Press.
- Wigley FM. Clinical practice. Raynaud’s phenomenon. N Engl J Med. 2002 Sep 26;347(13):1001–1008.
- Singh A, Ambujam S, Varghese A, et al. Salt-and-pepper appearance: A cutaneous clue for the diagnosis of systemic sclerosis. Indian J Dermatol. 2012 Sep;57(5):412–413.
- Gonin M, Gerster JC. Pigmentation disorders in systemic sclerodermia. Schweiz Rundsch Med Prax. 1994 Jan 11;83(2):42–45.
- Jimenez SA, Derk CT. Following the molecular pathways toward an understanding of the pathogenesis of systemic sclerosis. Ann Intern Med. 2004 Jan 6;140(1):37–50.
- Tan FK. Systemic sclerosis: The susceptible host (genetics and environment). Rheum Dis Clin North Am. 2003 May;29(2):211–237.
- Walker UA, Tyndall A, Czirják L, et al. Clinical risk assessment of organ manifestations in systemic sclerosis: A report from the EULAR Scleroderma Trials and Research group database. Ann Rheum Dis. 2007 Jun;66(6):754–763.
- Adelowo OO, Oguntona S. Scleroderma (systemic sclerosis) among Nigerians. Clin Rheumatol. 2009 Sep;28(9):1121–1125.
- Sharma VK, Trilokraj T, Khaitan BK, et al. Profile of systemic sclerosis in a tertiary care center in North India. Indian J Dermatol Venereol Leprol. 2006 Nov–Dec;72(6):416–420.

