Rheumatoid arthritis (RA) is a chronic systemic autoimmune inflammatory disease. Although RA develops its central pathology within the synovium of diarthrodial joints, many non-articular organs can be involved, particularly in patients with severe joint disease.1 Although most patients are asymptomatic, cardiac involvement is relatively common and includes rheumatic heart nodules, pericarditis (30–50%), pericardial effusion and conduction abnormalities.2,3 Cardiac tamponade due to rheumatoid pericarditis is considered rare and may present a diagnostic challenge.4
This article describes a case of 64-year-old man with a three-year history of rheumatoid arthritis who presented with rheumatoid pericarditis and cardiac tamponade physiology.
The Case
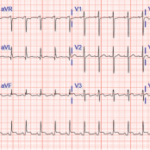
Mr. M is a 64-year-old man from El Salvador with a past medical history of type 2 diabetes mellitus, hypertension and seropositive RA, who presented to an outside hospital with acute-onset, left-sided chest pain. The chest pain was constant, progressively worsening, exacerbated with deep inspiration and relieved by lying flat and on his left side. He was noted to be tachycardic to 130–140s and his systolic blood pressure was in the 90s; an electrocardiogram showed ST elevation at I, AVL and V5–6. He was initially given thrombolytic therapy due to concern for acute coronary syndrome and transferred to our hospital for further management.
The patient was diagnosed with RA in 2015 when he presented with polyarticular joint pain. He was subsequently started on methotrexate, but he did not tolerate the medication well due to nausea and gastrointestinal discomfort. Subcutaneous adalimumab, 40 mg every two weeks, was added a month later; however, he stopped taking both medications a few weeks later because he felt “unwell.”
Upon arrival at our hospital, Mr. M underwent a left heart catheterization that revealed normal coronary arteries. Physical examination revealed a pulse of 134, respiration of 21, blood pressure of 108/75 and oxygen saturation of 93% on room air. No jugular venous distention was appreciated, and no friction rub was heard; however, muffled heart sounds and decreased breath sounds were noted. Synovitis was present in his right wrist, right second and third metacarpophalangeal joints, and left second metacarpophalangeal joints.
Laboratory data included elevated white blood cells at 20×103/mm3 (87% neutrophils, 7% lymphocytes and 6% monocytes), normocytic anemia (hemoglobin: 11.4 g/dL) and mild thrombocytosis (a platelet count of 479×103/mm3). The erythrocyte sedimentation rate was normal at 36, but the C-reactive protein was >190 mg/L. Rheumatoid factor was present at an elevated titer of 536 IU/mL and anti-citrullinated cyclic peptide antibodies were positive at 181 units. The patient tested negative for anti-nuclear antibodies. Human immunodeficiency virus was not detected, and the T-SPOT tuberculosis test was negative.
A chest X-ray showed moderate cardiomegaly and a tortuous aorta (see Figure 1, top right). A computed tomography angiogram revealed a moderate-size complex pericardial effusion (see Figure 2, bottom right). An echocardiogram showed moderate pericardial effusion with signs of tamponade.