Diagnosis & Treatment
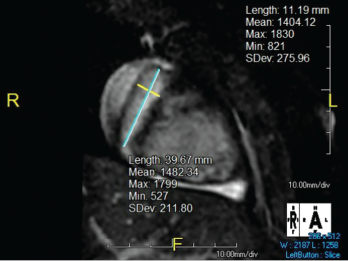
Figure 2. The right coronary artery sustained a giant fusiform aneurysm 11 mm in diameter (z-score = 20) and 40 mm in length.
The patient was diagnosed with granulomatosis with polyangiitis (GPA) and started on 1,000 mg of pulse dose intravenous methylprednisolone daily for three days and 81 mg daily of aspirin.
Sinus computerized tomography (CT) showed mucosal thickening and “bubbly” fluid in the sphenoid sinuses. A chest CT showed pleural effusions and potential upper lung nodules measuring 5 mm. A percutaneous biopsy of the left kidney revealed severe necrotizing crescentic pauci-immune glomerulonephritis.
Overall, this patient demonstrated severe manifestations of GPA equating to a validated Pediatric Vasculitis Activity Score (PVAS) of 34.1 Note that the current PVAS does not include scoring criteria for coronary artery aneurysms.1
Because of the severity of the renal disease, the patient was treated with 1 mg/kg/day methylprednisolone, 15 mg/kg of intravenous cyclophosphamide every two weeks for two doses and 375 mg/m2/week of rituximab for four weeks, a combination regimen consistent with the RITUXVAS trial.2 After four doses of rituximab, the patient denied any symptoms beyond mild rhinorrhea, and her renal disease gradually resolved.
Cardiac magnetic resonance imaging was performed, revealing giant aneurysms (see Figure 1, and Figure 2). The patient was subsequently started on warfarin and aspirin; she continues to have no cardiac symptoms. Continued management with rituximab as maintenance therapy is consistent with the MAINRITSAN trial.3 As of December 2020, the patient had a persistent PVAS of 2, secondary to residual valvular heart disease.
Discussion
Granulomatosis with polyangiitis is a small-vessel vasculitis associated with ANCA and multi-organ involvement.4 Aside from Kawasaki disease and IgA vasculitis, the systemic vasculitides are rare in the pediatric population, at an incidence of 0.24 per 100,000 children annually.1,5 Consequently, the average delay from symptom onset to diagnosis is 2.1 months, with a hospitalization rate 1.3 times that of adults.4,6
GPA typically presents with involvement of the upper and lower respiratory tracts, as well as renal manifestations, most commonly pauci-immune crescentic glomerulonephritis.5,7
The clinician who suspects or diagnoses an ANCA-associated vasculitis in a pediatric patient should consider coronary artery aneurysms as a possible & dangerous sequela.
Cardiac involvement in GPA is typically limited to venous thrombosis, as reported in three of 183 patients in the ARChiVe study.4 One reported case of coronary artery aneurysms in GPA, published in December 2010, involved a 25-year-old man who subsequently experienced an expansive anterior myocardial infarction and ventricular tachycardia necessitating electrical cardioversion.8 Cardiac involvement in GPA can also have confounding presentations. Varnier et al. described a 16-year-old boy with a tricuspid vegetation masquerading as infective endocarditis despite negative cultures and a positive PR3-ANCA.9
Our patient’s unique cardiac manifestations brought to the authors’ attention three significant considerations: