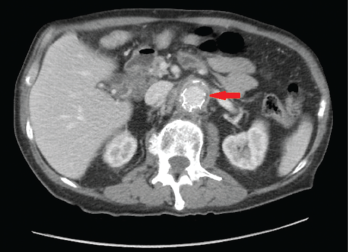
Figures 1A & 1B (below): A CT scan with abdominal and pelvic axial (a) and sagittal (b) views showing inflammatory changes (red arrow) adjacent to the aorta.
A 76-year-old Caucasian male with a history of abdominal aortic aneurysm repair five years earlier presented with three months duration of worsening periumbilical abdominal pain associated with nausea, non-bloody emesis, decreased appetite, fatigue and a 40 lb. weight loss. He denied having fever, chills, night sweats, temporal headaches, vision loss, chest pain, shortness of breath and jaw, upper and lower extremity pain.
On physical exam, the patient had no temporal artery tenderness. His peripheral pulses were normal and symmetric. The abdominal exam was significant for tenderness in the left periumbilical region with no guarding or rebound tenderness.
Laboratory analysis revealed a white blood cell count of 10.7 k/mm3, hemoglobin level of 11.1 g/dL and platelets at 294 k/mm3. The sedimentation rate of 140 mm/hr was elevated (normal: 0–22 mm/hr), as was the C-reactive protein level at 23.2 mg/L (normal: 2.0–8.0 mg/L). The creatinine level was normal at 0.93 mg/dL (normal: 0.6–1.50 mg/dL). The albumin level was low at 2.2 g/dL (normal: 3.4–5 g/dL).
A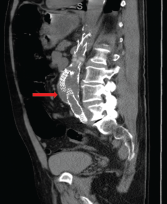 computed tomography (CT) scan of the abdomen and pelvis with contrast showed wall thickening and adjacent fat stranding involving the abdominal aorta and proximal bilateral common iliac arteries at the level of endovascular stent for the abdominal aortic aneurysm (see Figures 1a and 1b, right). These findings were suspicious for aortitis.
computed tomography (CT) scan of the abdomen and pelvis with contrast showed wall thickening and adjacent fat stranding involving the abdominal aorta and proximal bilateral common iliac arteries at the level of endovascular stent for the abdominal aortic aneurysm (see Figures 1a and 1b, right). These findings were suspicious for aortitis.
The patient was started on 40 mg intravenous methylprednisolone every eight hours. He experienced significant improvement in his abdominal pain and appetite.
A rheumatologist was consulted and recommended discontinuation of the methylprednisolone due to concern for infectious aortitis.
A vascular surgeon performed an aortic endograft explant and aortobiiliac bypass with CryoLife allograft. A large amount of pus surrounding the endograft was evident during surgery. The surgery was complicated by a splenic bleed requiring splenectomy. Histopathology revealed multiple necrotizing granulomas.
Aortic endograft cultures grew Coccidioides species. Serum Coccidioides complement fixation was positive 1:32 (normal <1:2) and (1-3)-β-d-glucan assay was elevated >500 pg/mL.
Initially, the patient was started on broad-spectrum anti-fungal coverage, with 375 mg isavuconazonium sulfate intravenously every eight hours. He received six doses. Then, he was switched to 375 mg isavuconazonium sulfate intravenously once daily with 5 mg/kg liposomal amphotericin B once daily. Once the mold was speciated to Coccidioides, the patient was taken off the isavuconazonium sulfate and switched to 400 mg intravenous fluconazole daily. The liposomal amphotericin B was continued for disseminated coccidioidomycosis.
The patient’s hospital course was complicated by retroperitoneal hematoma, prolonged ileus, hiatal hernia requiring exploratory laparotomy, acute renal failure requiring continuous renal replacement therapy, hemopneumothorax requiring chest tubes and acute respiratory failure requiring intubation. Unfortunately, his medical condition continued to deteriorate, and he died after transitioning to hospice care.