During the rheumatologic consultation at this presentation, the patient had a striking physical appearance, with prominent forehead creases (see Figure 1). According to the patient, these had developed within the past year or two. He had multiple joint effusions in the wrists and knees (see Figure 2). He had limited
range of motion in his left shoulder, elbows, wrists, knees and ankles. His range of motion was also limited with reduced flexion of his metacarpophalangeal joints (MCP) and proximal interphalangeal joints (PIP) on both hands and thickened fingers. He had edema and tenderness of the midfoot, as well as tenderness of the Achilles tendon on palpation (see Figure 2). No clubbing was noted on the examination, but he did have cutis verticis gyrata (i.e., thickening of his scalp).
Laboratory tests at this time revealed low ferritin levels. Fecal occult blood and fecal calprotectin were abnormal. His CRP and ESR were elevated. His IgG level was mildly elevated, but he had normal IgA and IgM levels. HLA-B27, cyclic citrullinated peptide (CCP), rheumatoid factor (RF) and anti-nuclear antibody (ANA) tests were negative.
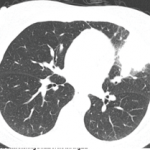
Magnetic resonance enterography (MRE) and X-ray of the sacroiliac (SI) joints were unremarkable. X-rays showed generalized osteopenia with periosteal reaction and sclerosis of both ulna (see Figure 3). He had small, suprapatellar effusions on both legs. Due to concern for both enthesitis-related juvenile idiopathic arthritis (ERA-JIA) and Crohn’s disease, he was started on 10 mg of oral methotrexate weekly and 40 mg of adalimumab via subcutaneous injection every two weeks.
He did not show much improvement on medication, and—given his striking physical examination, with forehead furrowing, and further literature searches—his case was reconsidered; his symptoms were found to be consistent with PDP.
Genetic testing was subsequently performed, revealing two heterozygous pathogenic variants in SLCO2A1.
Methotrexate was subsequently increased to 20 mg weekly, and he was switched from adalimumab to infliximab infusions due to his poor response and GI symptoms. Around the time his medications were changed, the patient started physical therapy, and dietary restrictions appropriate for patients with IBD were implemented. The patient responded to treatment, with improved knee effusions and pain. However, digit thickness continued to progress. Unfortunately, the patient developed antibodies to infliximab and the exclusionary diet was discontinued. Since then, his joint swelling and pachyderma have worsened.
Eventually, the patient was started on golimumab infusions at 100 mg every four weeks, along with subcutaneous 20 mg of methotrexate weekly. The patient experienced significant improvement in his arthritis. This improvement also coincided with utilization of a Crohn’s elimination diet, which further lowered his gastrointestinal inflammation.