The Case
A 35-year-old African American woman with a history of systemic lupus erythematosus (SLE) with multi-organ involvement presented with a three-month history of an intensely pruritic scaling rash on her scalp.
Prior to this encounter, the patient had a complicated medical course requiring multiple hospital admissions, leading to the diagnosis of Class V lupus nephritis, myositis, renal and pulmonary thrombi, microangiopathic hemolytic anemia and persistent discoid skin lesions (see Figures 1a and b). The patient’s medications for her SLE included prednisone 40 mg daily, hydroxychloroquine 400 mg daily and mycophenolate mofetil (MMF) 3 g/day. At the time of the patient’s initial diagnosis of SLE, her antibody profile revealed ANA 1:160 (speckled), anti-dsDNA negative, anti-SSA 274 EU/Ml, anti-Smith 165 EU/mL and anti-RNP 189 EU/mL.
Throughout the course of several admissions, she complained of a persistent pruritic skin rash, which initially started on her arms and hands, with hyperpigmentation, peeling and a psoriasiform appearance. The skin biopsy from the forearm performed at the time of the SLE diagnosis was consistent with a lupus rash. With initiation of immunosuppressive therapy, both her rash and pruritus significantly improved. However, at subsequent hospitalizations due to possible medication nonadherence and underlying disease activity, her SLE worsened, and she required several courses of pulse corticosteroids. There was temporary improvement in her skin findings, only to be followed by recurrence of her symptoms.


Over the course of these admissions, her rash worsened and became crusted, eventually spreading to involve her scalp (see Figures 2a and b). This was puzzling to the medical service and raised suspicion for an opportunistic infection (e.g., bacterial superinfection, rare fungal infections or herpes simplex virus) and a possible adverse drug reaction. She was empirically treated with antibiotics and antiviral agents, without notable improvement.
This was followed by selective discontinuation of the patient’s medications in an attempt to identify the culprit of a possible adverse drug reaction. It was found that the patient’s rash would improve with cessation of MMF and return once her therapy was resumed. This led to a strong suspicion that MMF was the source of the allergic type skin rash, which was causing the intense itching and scaling.
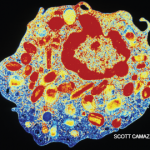
However, the diagnosis of scabies in several nurses in the ward prompted an evaluation of our patient for scabies. Microscopic analysis of scalp scrapings revealed hundreds of mites and scybala, consistent with a diagnosis of severe crusted scabies. The patient was treated with multiple doses of permethrin cream and ivermectin with resolution of the rash (see Figures 3a and b).