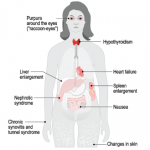
Figure 1
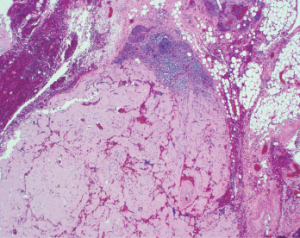
This image shows a lymph node with near-total replacement by amorphous amyloid material (H&E, 100x).
A 54-year-old African American man arrived at the emergency department with the acute onset of a tender mass on the left side of his neck. It had been getting progressively larger for the preceding two days.
History & Examination
His history included chronic right hip osteoarthritis with two surgeries performed five years prior. At his initial presentation, he noted increased fatigue the preceding few days, as well as generalized weakness and decreased appetite.
His habits included smoking a half-pack of cigarettes daily for 30 years, occasional alcohol consumption and avoidance of recreational substances. Because he had been employed by the oil industry working on scaffolding, he had traveled extensively throughout the U.S. for work, but he denied traveling outside the country or to regions where Lyme disease is known to be endemic.
On examination, he displayed a 4–5 cm non-pulsatile mass on the left side of his neck. It was moderately tender to palpation. He also had mild thyromegaly with a suggestion of thyroid nodules. His right hip was not tender and had no swelling, ecchymosis, warmth or erythema. Flexion of his hip was limited to 90º, and internal as well as external rotation was limited to approximately 15º.
Evaluation of laboratory tests revealed an elevated rheumatoid factor at 25 (upper limit of normal [ULN]: 14), and an elevated serum immunoglobulin G at 1,700 mg/dL (ULN: 1,600 mg/dL). Serum protein electrophoresis revealed a total gamma component elevation at 1.74 g/dL (ULN: 1.6 g/dL) with M-component elevation at 1.28 g/dL (ULN: 0 g/dL).

Dr. Bhavasar
A computed tomography (CT) scan with contrast of the patient’s neck revealed a large, mildly heterogeneous inferior left neck and left subclavicular mass, likely reflecting a large nodal conglomerate approximately 4.5 cm anteroposterior, 7.5 cm transverse and 7.5 cm in cranio-caudal dimensions. Portions were hypoattenuating relative to muscle, perhaps reflecting cystic or necrotic areas. Calcifications seen within the mass, in conjunction with an enlarged multinodular thyroid gland, were most worrisome for metastatic lymphadenopathy related to thyroid cancer. An X-ray of his right hip displayed total arthroplasty without evidence of acute complication.
Fine needle aspiration of the thyroid nodule noted on the CT scan was performed and found to be consistent with a lymphocytic (Hashimoto) thyroiditis. The neck mass was biopsied, and subsequent tissue studies revealed a Gram stain with very few white blood cells, no organisms and no acid-fast bacilli. A tissue culture did not result in growth of bacteria, yeast, fungi or mycobacteria at six weeks. The biopsy demonstrated lymph nodes and fibro-adipose tissue with extensive replacement by amorphous deposits of acellular material consistent with amyloid (see Figure 1, above right). A Congo red stain was positive for polarized apple-green birefringent material, confirming the impression of amyloid (see Figure 2, p. 38). Amyloid also involved vessel walls, and areas of ossification were present. The biopsy material subsequently underwent liquid chromatography tandem mass spectroscopy at Mayo Clinic Laboratories, which subtyped the amyloid as AL (lambda) type.