Conclusion
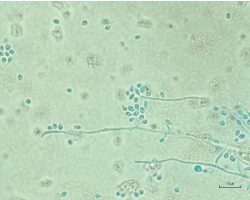
Figure 5. Light microscopy of aspirate culture showing Sporothrix schenckii species.
Although cognitive bias likely played a role in our patient’s initial care, the primary team’s systematic approach and early involvement of appropriate specialists helped prevent the significant delays and misdiagnosis often seen in opportunistic illnesses.
As rheumatologists, our role is not only to diagnose and treat rheumatologic disease, but also to consider alternate explanations and to advocate for thorough and appropriate work-up to reasonably exclude infectious etiologies.
Reducing the impact of cognitive bias in the care of our patients will likely necessitate increasing the available rheumatology workforce, and rheumatology educational opportunities during medical training and for our colleagues in practice.
Sarah Dill, MD, was a third-year rheumatology fellow at the University of Colorado, Aurora, when this article was written. She is now working at the Rocky Mountain Regional VAMC in Aurora, Colo.
Duane Pearson, MD, is an associate professor in the Department of Internal Medicine-Rheumatology at the University of Colorado.
References
- O’Sullivan E, Shofield S. Cognitive bias in clinical medicine. J R Coll Physicians Edinb. 2018 Sep;48(3):225–232.
- Graber ML, Franklin N, Gordon R. Diagnostic error in internal medicine. Arch Intern Med. 2005 Jul 11;165(13):1493–1499.
- Saposnik G, Redelmeier D, Ruff CC, Tobler PN. Cognitive biases associated with medical decisions: A systematic review. BMC Med Inform Decis Mak. 2016 Nov 3;16(1):138.
- Sharim R, Thomas P, Mathew L, et al. Perceptions of infection risk with immunomodulatory medications. J Clin Rheumatol. 2018 Mar;24(2):80–84.
- Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003Aug;78(8):775–780.
- Yamaguchi T, Ito S, Takano Y, et al. A case of disseminated sporotrichosis treated with prednisolone, immunosuppressants, and tocilizumab under the diagnosis of rheumatoid arthritis. Intern Med. 2012;51(15):2035–2039.
- Gottlieb GS, Lesser CF, Holmes KK, Wald A. Disseminated sporotrichosis associated with treatment with immunosuppressants and tumor necrosis factor-alpha antagonists. Clin Infect Dis. 2003 Sep 15;37(6):838–840.
- Chowdhary G, Weinstein A, Klein R, Mascarenhas BR. Sporotrichal arthritis. Ann Rheum Dis. 1991 Feb;50(2):112–114.
- Appenzeller S, Amaral TN, Amstalden EMI, et al. Sporothrix schenckii infection presented as monoarthritis: Report of two cases and review of the literature. Clin Rheumatol. 2006 Nov;25(6):926–928.
- Byrd DR, El-Azhary RA, Gibson LE, Roberts GD. Sporotrichosis masquerading as pyoderma gangrenosum: Case report and review of 19 cases of sporotrichosis. J Eur Acad Dermatol Venereol. 2001 Nov;15(6):581–584.
- Yang DJ, Krishnan RS, Guillen DR, et al. Disseminated sporotrichosis mimicking sarcoidosis. Int J Dermatol. 2006 Apr;45(4):450–453.
- White M, Adams L, Phan C, et al. Disseminated sporotrichosis following iatrogenic immunosuppression for suspected pyoderma gangrenosum. Lancet Infect Dis. 2019 Nov;19(11):e385–e391.
- Isa-Isa R, García C, Isa M, Arenas R. Subcutaneous phaeohyphomycosis (mycotic cyst). Clin Dermatol. 2012 Jul–Aug;30(4):425–431.
- Sheikh SS, Amr SS. Mycotic cysts: Report of 21 cases including eight pheomycotic cysts from Saudi Arabia. Int J Dermatol. 2007 Apr;46(4):388–392.
- Queiroz-Telles F, Buccheri R, Benard G. Sporotrichosis in immunocompromised hosts. J Fungi (Basel). 2019 Jan 11;5(1):8.
- Mahajan VK. Sporotrichosis: An overview and therapeutic options. Dermatol Res Pract. 2014;2014:272376.
- de Lima Barros MB, de Almeida Paes R, Schubach AO. Sporothrix schenckii and sporotrichosis. Clin Microbiol Rev. 2011 Oct;24(4):633–654.
- Gotzsche PC, Johansen HK. Short-term low-dose corticosteroids vs placebo and nonsteroidal antiinflammatory drugs in rheumatoid arthritis. Cochrane Database Syst Rev. 2004;2005(3):CD000189.
- Svensson B, Boonen A, Albertsson K, et al. Low-dose prednisolone in addition to the initial disease-modifying antirheumatic drug in patients with early active rheumatoid arthritis reduces joint destruction and increases the remission rate: A two-year randomized trial. Arthritis Rheum. 2005 Nov;52(11):3360–3370.
- Stuck AE, Minder CE, Frey FJ. Risk of infectious complications in patients taking glucocorticosteroids. Rev Infect Dis. 1989 Nov–Dec;11(6):954–963.
- Dixon WG, Suissa S, Hudson M. The association between systemic glucocorticoid therapy and the risk of infection in patients with rheumatoid arthritis: Systematic review and meta-analyses. Arthritis Res Ther. 2011Aug 31;13(4):R139.
- Dixon WG, Abrahamowicz M, Beauchamp M-E, et al. Immediate and delayed impact of oral glucocorticoid therapy on risk of serious infection in older patients with rheumatoid arthritis: A nested case-control analysis. Ann Rheum Dis. 2012 Jul;71(7):1128–1133.
- Migita K, Arai T, Ishizuka N, et al. Rates of serious intracellular infections in autoimmune disease patients receiving initial glucocorticoid therapy. PLoS One. 2013 Nov 19;8(11):e78699.