This case highlights an unprovoked massive pulmonary embolism in a young patient with Behçet’s disease. A paucity of literature addresses pulmonary manifestations of Behçet’s, and the prognosis, morbidity and mortality involved with this patient population.
Behçet’s is an autoimmune disease commonly presenting with recurrent oral and genital ulcers, as well as skin and eye involvement. Because Behçet’s does not have pathognomonic findings limited only to its own disease process, the diagnosis is made using criteria established by the International Study Group for Behçet’s Disease in 1990. The criteria emphasize recurrent oral and genital ulcers, as well as eye lesions, skin lesions and a positive pathergy test. A positive pathergy test stands as a unique disease feature, showcasing immune system hyper-reactivity and signals, and upregulated inflammatory response. Patients are typically in the second to third decade of life at onset with an equal male to female predominance. Younger age of onset and male sex are markers of more severe disease.
The etiology of this disease is not well understood, and vascular involvement is thought to be due to inflammation localized to the vasa vasorum. Neutrophil activation and migration in conjunction with free radical generation have been proposed as the underlying mechanism. More recent studies suggest a role of T lymphocyte upregulated immune response as an important part of disease pathogenesis. Clinically active disease has been associated with oligoclonal T cell expansion. An increased T cell response has been shown against peptides derived from heat shock proteins, leading to the theory that heat shock proteins are activating antigens in Behçet’s. Streptococcal and herpes simplex virus have also induced a T cell proliferative response, further complicating the underlying etiology with an antimicrobial theory.
Vascular involvement occurs in up to 40% of patients with a male predisposition. Thrombosis is usually secondary to underlying vasculitis, with lower extremity venous thromboembolism presenting as the most common vascular abnormality in patients with Behçet’s. Multiple studies have tried to establish a genetic link between the development of BD and HLA-B51 positivity; however, results have thus far been controversial. In Turkey, the risk of disease development with this allele is 13.1% compared to 1.3% in the U.S. It has been proposed that individuals with HLA-B51 positivity tend to run a more refractory symptom course; however, this has been only been observational.
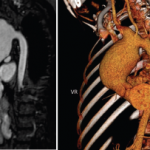
The pulmonary manifestations of this disease are uncommon. The pulmonary arteries are the second most common area of arterial involvement, with the aorta being first. Arterial aneurysms, venous thrombosis, pulmonary infarction, pulmonary vessel inflammation and reactivity and organizing pneumonias are known pulmonary complications. The true prevalence of pulmonary involvement in Behçet’s is unknown.