Putting the entire clinical picture together, I was most concerned for malignancy. Vasculitis seemed possible, although giant cell arteritis (GCA) seemed more consistent with her symptoms than did small vessel vasculitis. The muscle weakness was concerning for possible inflammatory myositis, but her normal transaminases placed this lower on the differential. The leg swelling and calf pain were concerning for deep vein thrombosis in the setting of an underlying inflammatory process.
At the end of the visit, a chest X-ray and further labwork were performed, and an urgent temporal artery ultrasound and Doppler ultrasound of the legs were ordered. The chest X-ray was remarkable for apical scarring, basilar atelectasis and/or scarring, bronchiectasis in the lingula and absence of lymphadenopathy (see Image 1). The radiographic differential diagnosis included interstitial lung disease (ILD), lymphoma and prior tuberculosis. Labwork revealed normal CK (34) and aldolase (5.3), urinalysis without protein and with 5 RBC, 0 WBC, and no casts, positive pANCA (MPO and PR3 pending), negative ANA, SPEP without M-spike, and elevated total IgG (3082). Doppler ultrasound of the legs was negative for deep vein thrombosis.
With the chest X-ray and these results in hand, microscopic polyangiitis (MPA) with pulmonary involvement, ILD and lymphoma were at the top of my differential.
Giant cell arteritis now seemed less likely with the pulmonary abnormalities (although underlying/undiagnosed ILD and new-onset GCA was a possibility). We referred her urgently to nephrology clinic for evaluation, scheduled a chest CT and cancelled the temporal artery ultrasound. The consulting nephrologist noted no dysmorphic RBCs or cellular casts in the urinalysis, and the spot urine protein-to-creatinine ratio was normal (0.17). Based on these findings, glomerulonephritis was not suspected.
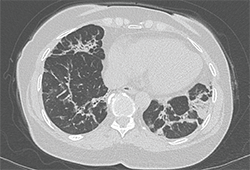
Image 2: The chest CT revealed abnormalities in the bases and lingula, with bilateral mild bronchiectasis, consolidative opacities and fibrosis.
The chest CT revealed abnormalities in the bases and lingula, with bilateral mild bronchiectasis, consolidative opacities and fibrosis (see Image 2). The appearance was concerning for cryptogenic organizing pneumonitis or resolving pneumonia, and did not have features typical of ANCA vasculitis or idiopathic pulmonary fibrosis.
A week after the CT scan was performed, her MPO ELISA returned highly positive (316), and PR3 was normal (1).
During a return clinic visit, her oxygen saturation dropped to 87% on room air during a six-minute walk test. A transthoracic echocardiogram showed normal left and right ventricular size and function, and normal pulmonary pressure.
At this point, she was clinically stable and had not received empiric corticosteroid treatment. A lung biopsy would be necessary to diagnose the underlying pulmonary process, and she was urgently referred to thoracic surgery clinic. The thoracic surgeon scheduled a video-assisted thoracoscopic surgery (VATS) to obtain biopsies from the right upper, middle and lower lobes. Given that the thoracic musculature would be exposed during the operative approach, he also planned to perform a serratus muscle biopsy in addition to the lung biopsies, in order to (in his words) “cover all the bases.”

