Her lung biopsy specimens captured multiple small arteries, around which was no evidence of inflammation or vessel wall necrosis. Fibrosis, bronchiectasis, germinal centers in lymphoid aggregates and bronchiolocentric inflammation were seen in the lung base and middle lobe (see Image 3). The upper lobe alveoli were relatively spared and were surrounded by chronic inflammatory infiltrates in the interstitium and pleura.
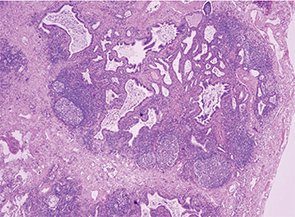
Image 3: The lung biopsy revealed fibrosis, bronchiectasis, germinal centers in lymphoid aggregates and bronchiolocentric inflammation in the lung base and middle lobe.
This patient’s case was discussed at a Pulmonary Pathology conference and was thought to be consistent with ILD, without features of vasculitis or pulmonary hemorrhage.
On the basis of constitutional symptoms, active pulmonary inflammation with B cell germinal centers, and pANCA with MPO, we decided to start treatment with both high-dose oral steroids (1 mg/kg/day) and rituximab.
Which Came First, the ILD or the ANCA?
After reviewing the lung biopsy pathology, it was time to step back and reconsider her case. The workup had been incited by a positive pANCA (later confirmed by high MPO) in the setting of constitutional symptoms, but without focal symptoms of vasculitis other than initial cough and mild dyspnea on exertion. Now, her chest imaging and lung biopsy indicated ILD with active inflammation and fibrosis, but no histologic evidence of small vessel vasculitis.
Dyspnea was a minor component of this patient’s symptoms. Her exercise tolerance had only diminished at the start of her febrile illness in December; before then, she could walk several miles. After the abnormal chest X-ray result during her first visit, the patient’s daughter called me to share that her mother had been diagnosed with a “lung problem” seven years before in the Dominican Republic, but never received treatment for it. The daughter confirmed that her mother had no difficulty breathing until the start of this most recent illness.
The patient’s presentation raised several questions about the pathogenesis of her disease, whose answers could influence the treatment approach. Was this ILD, with an incidentally positive ANCA? After all, the fibrosis on lung biopsy suggested a chronicity of many months (more than the two months during which she had felt ill), if not years. Or was this a new case of MPA with lung fibrosis and bronchiectasis, rather than the expected small artery vasculitis and capillaritis?
Several observational studies and case series have assessed the relationship of ILD and ANCA, addressing different facets of the relationship:
- How often is ILD present in patients with ANCA vasculitis? Arulkumaran et al addressed this question in a retrospective chart review of 510 patients treated for ANCA vasculitis in a nephrology clinic.1 Thirty-eight percent carried a diagnosis of MPA and 62% had granulomatosis with polyangiitis (GPA) or eosinophilic granulomatosis with polyangiitis (EGPA). Among the entire cohort, 2.7% had ILD—defined as characteristic CT scan findings and/or lung biopsy results—either at initial vasculitis presentation or later in the course of disease. All cases of ILD occurred in patients with MPA (7.2% of MPA patients); ILD was not detected in any patients with GPA or EGPA. Among MPA patients there was no survival difference based on the presence versus absence of ILD.
- How often is ANCA detected in patients with known lung disease? Among 504 patients with idiopathic pulmonary fibrosis (IPF), 7.2% tested positive for ANCA (4% MPO and 3.2% PR3) at the time of first evaluation in the pulmonology clinic, in the absence of signs of vasculitis.2 Half of the patients had serial ANCA measurements, 11% of whom later developed a positive ANCA (5.7% MPO, 5.3% PR3). A clinical diagnosis of microscopic polyangiitis developed in 25% of those patients with a positive MPO-ANCA.
- What types of pulmonary pathology are seen in patients with ANCA vasculitis and pulmonary abnormalities? A case series reported pathology results among 27 patients with ANCA vasculitis (14 with MPO, 12 with PR3, one negative for both) that had undergone lung biopsy.3 Vascular lesions (78%) and interstitial abnormalities (74%) were the most common pathologic findings. Capillaritis was the most common vascular abnormality. Interstitial lesions were most frequently fibrosis, chronic inflammation, and necrotizing granulomas. Airway lesions were less common (41%) than interstitial and vascular lesions, and included bronchiolitis obliterans, necrotizing granulomas, and non-granulomatous inflammation. Usual interstitial pneumonia (UIP) diagnosed by radiographic or pathologic criteria was the most common finding in a series of patients with pANCA/MPO-ANCA-positive microscopic polyangiitis and lung fibrosis; in most cases, UIP preceded the diagnosis of MPA (Ulrich Specks, MD, personal communication).
In this patient’s case, we suspected that her ILD predated the onset of fevers in December, given the fibrotic component. We could not know when the ANCA had first developed, either with the initial onset of ILD or more recently. What we did know is that her fevers, weakness and calf pain greatly improved after starting high-dose oral steroids, soon followed by rituximab.

