Discussion
Castleman disease is a non-neoplastic lymphoproliferative disorder that arises from the clinicopathologic intersection of hematology, oncology, rheumatology and virology.
Unicentric Castleman disease involves a single lymph node station, whereas multicentric Castleman disease (MCD) involves multiple lymph node stations.
HHV-8, occurring most commonly in HIV-infected individuals, is a major driver of MCD, in which viral interleukin (IL) 6 creates a proinflammatory state. In HHV-8-negative MCD, also known as idiopathic MCD (iMCD), the exact etiologies are unknown, but excessive human IL-6 from germinal centers is a pathological driver.
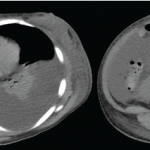
The iMCD diagnostic criteria consist of major criteria, which include multicentric lymphadenopathy and histopathologic lymph node features, such as regressed germinal centers, follicular dendritic cell prominence, vascularity or plasmacytosis. Minor criteria include elevated inflammatory markers, anemia, thrombocytopenia, hypoalbuminemia, renal dysfunction, polyclonal hypergammaglobulinemia, constitutional symptoms, hepatosplenomegaly, anasarca, cherry hemangiomatosis and lymphocytic interstitial pneumonitis. Exclusion criteria include infections, malignant/lymphoproliferative disorders and autoimmune/autoinflammatory diseases, notably SLE.1
Our patient met both major criteria and nine of the 11 minor diagnostic criteria for iMCD. She had a high-titer ANA and hypocomplementemia, but she did not have any lupus-specific autoantibodies or mucocutaneous manifestations of lupus, and her renal, neurologic, hematologic and constitutional manifestations were nonspecific and better explained by iMCD with macrophage activation syndrome.
There are reports of individuals with iMCD that initially mimicked SLE; in one case a patient similarly presented with heterogenous clinical manifestations, nephrotic syndrome and renal biopsy with negative immunofluorescence.2
There are also reports of individuals with SLE and Castleman-like features; in two cases, the Castleman-like features were noted on histological examination of lymph node biopsy, and the patients responded sufficiently to hydroxychloroquine and prednisone.3,4
Conclusion
Although the difference between primary iMCD mimicking SLE vs. SLE with Castleman-like features may be subtle, the correct diagnosis is likely to impact management, and recognition of iMCD in this case led to selection of an IL-6 inhibitor, siltuximab.5 This case underscores the importance of re-evaluating the diagnosis when a patient does not respond to initial treatment. Just as the microscopic examination of histopathology is crucial to the diagnosis, a microscopic examination of clinical details is paramount to the care of the patient. This is the art of medicine.
 Philip Chu, MD, RhMSUS, is a rheumatologist at Duke University Hospital, Durham, N.C., with an interest in musculoskeletal ultrasound.
Philip Chu, MD, RhMSUS, is a rheumatologist at Duke University Hospital, Durham, N.C., with an interest in musculoskeletal ultrasound.
 Mithu Maheswaranathan, MD, is a third-year rheumatology fellow in the Division of Rheumatology at Duke University School of Medicine, Durham, N.C., with interests in health literacy in rheumatic diseases and patient education. [Twitter: @MithuRheum]
Mithu Maheswaranathan, MD, is a third-year rheumatology fellow in the Division of Rheumatology at Duke University School of Medicine, Durham, N.C., with interests in health literacy in rheumatic diseases and patient education. [Twitter: @MithuRheum]