Differential diagnoses of lepromatous leprosy, tuberculosis, relapsing polychondritis and medium vessel vasculitis were entertained.
The patient’s complete blood count (CBC), RF, liver function, urine routine/microscopy (R/M), post-anterior chest X-ray, whole abdomen ultrasound and two-dimensional echocardiogram tests were within normal limits. He had raised inflammatory markers (C-reactive protein [CRP]: 5.32 mg/dL [upper limit of normal (ULN): 0.3] and erythrocyte sedimentation rate [ESR]: 49 mm/hour [ULN: 15]). Anti-nuclear antibody (ANA), rheumatoid factor (RF), anti-cyclic citrullinated peptide (CCP) antibody and anti-neutrophilic cytoplasmic antibody (ANCA) screening were negative. An infectious workup, consisting of blood culture, urine culture, viral markers and Mantoux tuberculin skin test, was negative.
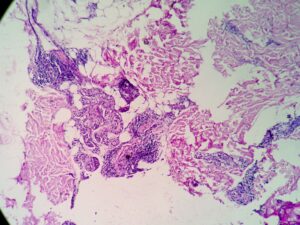
A skin biopsy of the hypopigmented macules revealed septal panniculitis without vasculitis (see Figure 5), but Fite-Faraco staining for acid fast organisms was negative, as was a slit skin smear from the ear lobule.
An inguinal ultrasound suggested necrotic inguinal lymph nodes, with excisional biopsy revealing collections of foamy histiocytes (i.e., lepra or Virchow cells) interspersed with lymphocytic infiltrates. Fite-Faraco staining highlighted globi of acid fast bacilli (Mycobacterium leprae) within and around the foamy histiocytes (see Figures 6 & 7). Lymph node cartridge-based nucleic acid amplification test (CBNAAT) didn’t detect Mycobacterium tuberculosis bacilli, ruling out tuberculosis, which is a close differential of leprosy.
A diagnosis of lepromatous leprosy with type 2 lepra reaction was made, with components including neuritis/nerve thickening, normoaesthetic hypopigmented macules, erythema nodosum, inflammatory polyarthritis, cartilage inflammation, episodic orchitis and tender lymphadenopathy.
The patient was started on multidrug therapy for multi-bacillary leprosy (MDT-MB) because he had more than five skin lesions and more than one nerve thickening. MDT-MB comprises dapsone, rifampicin and clofazimine. The treatment duration was planned for one year. High-dose glucocorticoids (i.e., 1 mg/kg of prednisolone) for type 2 lepra reaction was also prescribed.
At one month follow-up, the patient had recurrence of erythema nodosum lesions and auricular and nasal chondritis due to rapid tapering of glucocorticoids, so prednisolone and clofazimine doses were increased and MDT-MB was continued. His symptoms completely resolved and didn’t recur on further follow-up visits.
Discussion
This case report describes a case of lepromatous leprosy masquerading as relapsing polychondritis.
Leprosy, also known as Hansen’s disease, is a chronic granulomatous disease caused by M. leprae, which primarily affects the skin and peripheral nerves.1 However, it can affect nearly all organs and organ systems, with long-term complications and significant morbidity and mortality, thus requiring prompt diagnosis and treatment. Leprosy still occurs in over 120 countries but remains particularly endemic to Southeast Asia, with more than 10,000 cases reported in 2019 in each of India and Indonesia.2