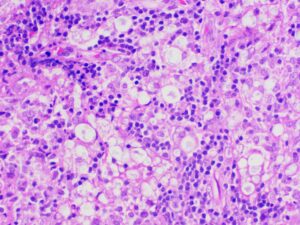
Figure 6: Lymph node biopsy shows foamy macrophages interspersed with lymphocytic infiltrates (lepra or Virchow cells).
Autoimmune diseases are characterized by multi-system manifestations, so it is important to rule out chronic infections, such as tuberculosis, leprosy and fungal infections, because the treatments for infections and autoimmune diseases are opposing, with the latter requiring glucocorticoids and immunosuppression and the former requiring antibiotics (and worsening with immunosuppressants). Particularly given the low sensitivity of many diagnostic tests for indolent infections, a high level of suspicion is needed when environmental or occupational histories suggest a higher risk for certain infections.
Our case highlights the importance of looking for chronic infections, such as leprosy, as mimics of AIRDs, such as relapsing polychondritis in this particular scenario.
Complete ear involvement occurs in leprosy in the form of painless, infiltrative nodular lesions of the pinna, with characteristic involvement of the ear lobule because the M. leprae has a predilection for involvement of cooler body sites.3 However, our case presented as painful auricular chondritis, sparing the lobule, which is a characteristic feature of relapsing polychondritis, and leading to the initial incorrect diagnosis.
Tender lymphadenopathy, nerve thickening and skin lesions were oddities in our case, which hinted at leprosy, an age-old mimic of autoimmune disease. The skin biopsy revealed septal panniculitis without vasculitis, with negative Fite-Faraco staining and slit skin smear. Despite that, a high suspicion of leprosy remained. Hence, the tender inguinal lymph node was targeted, which revealed the foamy histiocytes and globi of M. leprae on Fite-Faraco staining, clinching the diagnosis.
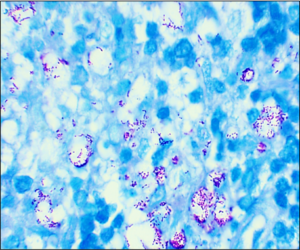
Figure 7: Lymph node biopsy Fite-Faraco staining shows globi of M. leprae bacilli. (Click to enlarge.)
Skin biopsy and slit skin smear have a low sensitivity of around 49–70% and 50%, respectively, for a diagnosis of leprosy.4 Gupta et al. did a histopathological study of lymph nodes in 43 cases of leprosy and showed that lymph nodes, if present, can show M. leprae in 92.2% of cases.5 Thus, a clinician should try to get a tissue or microbiological diagnosis, which at times may require repeated attempts at tissue sampling, as in our case.
A thorough history and systemic examination are crucial even in the modern world of advanced diagnostics. Appropriate tissue biopsy should be targeted for definitive diagnosis. One should actively rule out infection before diagnosing an AIRD because the treatments are diametrically opposite.


