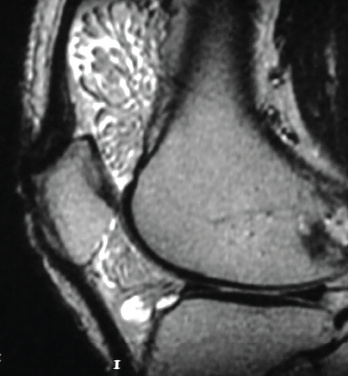
Figure 1. The MRI shows lipoma arborescens of the knee.
Given the minor swelling and the chronic, recurrent nature of the patient’s symptoms, joint aspiration and uric acid levels were deferred and imaging studies were ordered. An X-ray of his right knee demonstrated a small, suprapatellar joint effusion and nonspecific soft tissue swelling overlying the medial aspect of the knee, as well as edema within Hoffa’s fat pad, scattered vascular calcifications, mild narrowing of the medial compartment, mild subchondral sclerosis, minimal spurring of the tibial spines and no evidence of chondrocalcinosis.
At this point, a magnetic resonance imaging (MRI) scan of the knee was recommended. It demonstrated moderate joint effusion with lipoma arborescens (see Figure 1). A diagnosis of lipoma arborescens of the knee was made, and an orthopedic surgeon was called to further manage the patient.
The surgeon agreed with the diagnosis and administered a steroid injection into the joint for pain relief. Eventual joint replacement and synovectomy were scheduled, and the patient was discharged for follow-up.
Discussion
Given its uncommon nature, lipoma arborescens is rarely recognized as a potential cause of progressive and persistent joint swelling and pain. Diagnosis can be made with an MRI of the affected joint, sparing patients unnecessary examinations and procedures.
Johandi et al. demonstrate the utility of MRI in a similar clinical scenario involving a 51-year-old man presenting with unilateral knee pain and swelling and more than one year of misdiagnoses and unnecessary treatments.9 The patient described by Johandi et al. received plain radiographs at his initial visit and was subsequently diagnosed with degenerative osteoarthritis. He later presented with new-onset, bilateral, polyarticular arthritis of the wrist and metacarpophalangeal and proximal interphalangeal joints, in addition to persistent right knee pain and swelling. With normal lab findings and sterile fluid on knee joint aspiration, the patient’s diagnosis was changed to inflammatory oligoarthritis, and he was started on prednisolone and sulfasalazine therapy. Only after being referred to an orthopedic surgeon for synovectomy to rule out synovial tuberculosis was an MRI of the knee performed, which definitively pointed to a diagnosis of lipoma arborescens of the knee.
Given its uncommon nature, lipoma arborescens is rarely recognized as a potential cause of progressive & persistent joint swelling & pain.
Chronic joint pain and swelling can be challenging to diagnose and manage, and frustrating for patients experiencing the symptoms without a definitive solution. Both the above case presentation and the case described by Johandi et al. are complicated in that each patient had presented with a history of chronic polyarticular joint pain.
Supporting the hypothesis that lipoma arborescens is largely due to a reactive process, Vilanova et al. found that most patients present with symptoms suggestive of meniscopathy and are found to have degenerative joint changes and meniscal tear.8 Therefore, a reasonable degree of suspicion should be maintained for patients with such clinical signs and symptoms. Fortunately, the patient we have described was not exposed to unnecessary medical management, and diagnosis was made with MRI.
In Sum
The importance of including lipoma arborescens in the initial evaluation of patients with chronic, unremitting joint pain and swelling is demonstrated in the case above. A simple MRI provides a definitive diagnosis and synovectomy allows relief of patient symptoms. The etiology of this condition remains unknown; however, in many cases it is associated with such conditions as degenerative joint disease, popliteal cysts in approximately 20% of reported cases, diabetes mellitus, rheumatoid arthritis and psoriatic arthritis, suggesting the possibility of lipomatosis as the result of a reactive process.7,8,10 Primary disease is exceedingly uncommon.10
Patients often present with chronic and progressive joint swelling, limited range of motion and pain of the affected joint. Therefore, clinicians should be more suspicious of lipoma arborescens in patients with a presentation similar to the above case and a history consistent with degenerative joint disease, rheumatoid arthritis or other disease that could potentially fuel the reactive lipomatosis process.
Given the broad differential diagnosis, including pigmented villonodular synovitis, malignancy, synovial chondromatosis and rheumatoid arthritis, it is undoubtedly important to first rule out other rheumatic disease states and inflammatory arthropathies that can be acted upon. However, once initial diagnostics don’t provide an explanation for underlying symptomatology, clinicians should consider investigation with MRI; it is the gold standard for diagnosing lipoma arborescens.
In patients with this condition, an MRI will demonstrate a synovial mass of villous architecture depicting isointensity with subcutaneous fat. The mass is hyperintense on T1, but the signal is abolished in the sequences with fat saturation.11 There is no contrast uptake by the lesion, which excludes other inflammatory or neoplastic processes of the synovia.12 Therefore, MRI appearance of fatty synovial proliferation without other signal intensities within the lesion allows for a specific preoperative diagnosis.8
If the clinical picture is complicated and MRI does not shed light on the diagnosis, biopsy can be pursued. Histologic evaluation will show synovial hyperplasia and hypertrophy, with replacement of a significant amount of subsynovial tissue with mature adipocytes.8
The mainstay of treatment is synovectomy and, in primary disease, early intervention may be associated with decreased development of osteoarthritis.10,13 Current studies indicate a very low rate of recurrence.10
By acknowledging lipoma arborescens as a potential etiology of recurring joint pain and swelling, patients can be spared unnecessary diagnostics, empiric therapies and interventions aimed at managing more common arthropathies, and avoid progressive joint degeneration.13
 John Nawrocki, MD, completed an undergraduate degree in biology with a minor in biochemistry from Wilkes University, Wilkes-Barre, Pa., and medical school training at Geisinger Commonwealth School of Medicine, Scranton, Pa. His current research interests include immunology, hematology and oncology.
John Nawrocki, MD, completed an undergraduate degree in biology with a minor in biochemistry from Wilkes University, Wilkes-Barre, Pa., and medical school training at Geisinger Commonwealth School of Medicine, Scranton, Pa. His current research interests include immunology, hematology and oncology.
 Kevin Hess, DO, completed undergraduate degrees at Sacred Heart University, Fairfield, Conn., in cellular/molecular biology and biochemistry and his medical education at Rowan University School of Osteopathic Medicine, Stratford, N.J. He is a third-year internal medicine resident at ChristianaCare in Newark, Del. Current research interests include hematology and oncology.
Kevin Hess, DO, completed undergraduate degrees at Sacred Heart University, Fairfield, Conn., in cellular/molecular biology and biochemistry and his medical education at Rowan University School of Osteopathic Medicine, Stratford, N.J. He is a third-year internal medicine resident at ChristianaCare in Newark, Del. Current research interests include hematology and oncology.
Maryah Mansoor, MBBS, is a rheumatologist at Christiana Care Health System with special interest in scleroderma, lupus, myositis and ANCA-associated vasculitis.