Syphilis, an ancient disease caused by the spirochete Treponema pallidum, has been historically referred to as the great mimicker given its heterogenous presentation. Both systemic lupus erythematosus (SLE) and syphilis can have multi-systemic involvement. Both parvovirus B19 and syphilis have been reported to cause histologic features similar to those seen in lupus nephritis.
We present a case in which co-infection with syphilis and parvovirus B19 could have been mistaken for lupus nephritis. We highlight clinical features to help differentiate between lupus nephritis and nephrotic syndrome caused by co-infection with syphilis and parvovirus B19. Making the correct diagnosis has important implications: Nephrotic syndrome associated with parvovirus B19 often improves spontaneously and that with syphilis improves with penicillin, whereas lupus nephritis requires systemic immunosuppression.
Case Presentation
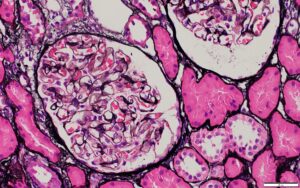
A 34-year-old Angolese man presented with lower extremity edema, headache, malaise, arthralgias, rash, diarrhea and chest pain of six weeks’ duration. He previously was evaluated at an urgent care clinic and was prescribed an oral non-steroidal anti-inflammatory drug for chest pain and myalgias, with symptomatic improvement. Renal biopsy was concerning for classes II and V lupus nephritis, for which a rheumatologist was consulted.
His creatinine was 1.4 mg/dL (reference range [RR] 0.75–1.20 mg/dL for men) on admission. Liver function tests were normal, except for an isolated elevation in alkaline phosphatase confirmed to be of hepatic etiology, with a corresponding elevation in gamma-glutamyl transferase.
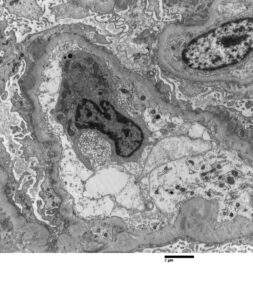
FIGURE 2: ELECTRON MICROSCOPY
Rare subepithelial and mesangial immune complex mediated type electron dense deposits present. Moderate podocyte epithelial foot process effacement is shown.
(Click to enlarge.)
The patient had recently been diagnosed with syphilis and treated with intramuscular penicillin a few weeks prior to his admission. His medical history included a prior diagnosis of COVID-19 and a remote history of malaria. Neither he nor his family had any history of autoimmune disease. He had not been taking any regular medications prior to admission. He denied use of illicit substances and had no travel outside the U.S. in several years. He reported being sexually active with male partners.
On admission to our hospital, his exam revealed prominent bilateral axillary and bilateral inguinal lymph nodes, soft tissue swelling in both ankles and pretibial pitting edema. Examination found no appreciable rashes on the skin, including a normal genital exam with no ulcerative lesions. The patient denied malar rash, photosensitivity, Raynaud’s phenomenon, history of venous thromboembolic events, dry mouth, dry eye, history of seizure or stroke, history of cytopenias, nasal or oral ulcers, or hair loss.