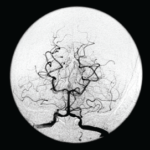
Figure 1A
A magnetic resonance angiogram (MRA) of the head/neck showed no high-grade stenosis, focal occlusion or aneurysm. A 2D echocardiogram showed a normal ejection fraction at 60–65% with diastolic dysfunction and no evidence of masses, thrombi or vegetations.
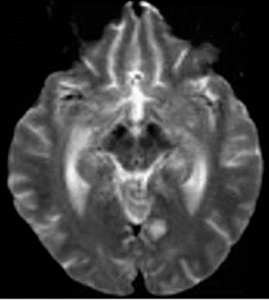
Figure 1B
An ultrasound of the carotid arteries showed 1–39% stenosis of the right and left internal carotid artery, with mild homogeneous plaque.
The patient was started on dual antiplatelet therapy and a statin, and her care was then transferred to the stroke team for continued workup.
The patient’s mental status deteriorated during admission. She became disoriented to questioning and eventually lost the ability to speak, swallow and walk.
Laboratory tests revealed: erythrocyte sedimentation rate of 102 mm/hour (normal: 0–20 mm/hour), C-reactive protein of 1.7 mg/L (normal: <8.2) and hemoglobin of 10.4 mg/dL (normal: 12.0–16.0 mg/dL). The white blood cell count was normal at 8,310/uL (normal: 3,900–12,700/uL), as were her platelets at 250,000/uL (normal: 150,000–350,000/uL). Liver function tests and blood glucose levels were normal. Her creatinine was 3.7 (baseline 2.2), with a glomerular filtration rate of 17 mL/min/1.73 m2 (normal: >60 mL/min/1.73 m2).
She had a Glasgow Coma score (GCS) of 9 (eye opening, 4; verbal response, 1; motor response, 4) and global aphasia with no usable speech or auditory comprehension. Decerebrate posturing was noted during the exam.
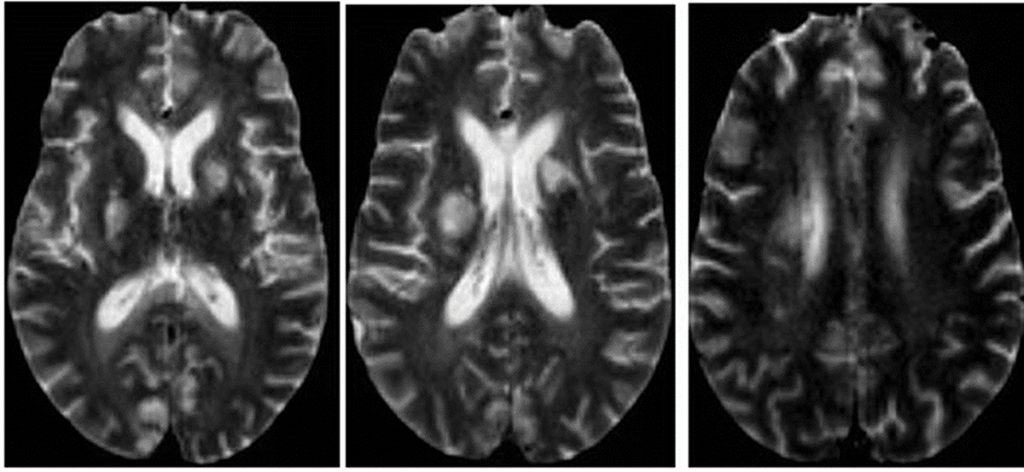
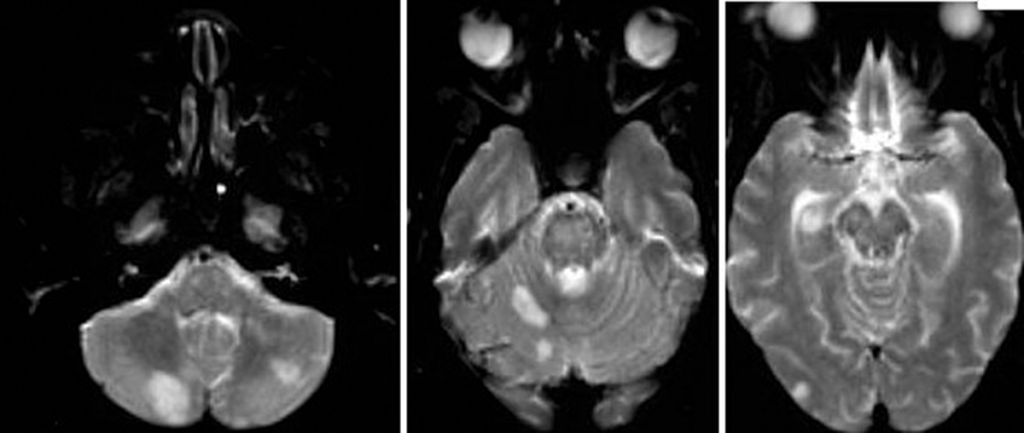
Figure 2: An MRI of the brain without contrast.
Further tests were performed, including an electroencephalogram (EEG), which was abnormal with generalized slowing indicative of a marked, diffuse, nonfocal and nonspecific encephalopathy. An interventional radiology cerebral angiogram was conducted and showed multifocal areas of distal intracranial artery narrowing, suggestive of vasculitis (see Figures 3 and 4).
A rheumatologist was consulted to evaluate the patient for central nervous system (CNS) vasculitis.
The patient developed acute hypoxic respiratory failure and experienced a febrile episode. She was subsequently intubated and started on broad-spectrum antibiotics (vancomycin and piperacillin/tazobactam). A sputum culture grew Citrobacter werkmanii, which was treated with a seven-day course of piperacillin/tazobactam.
Further lab test results: ANCA was normal (<1:20); MPO-ANCA was 2 units (normal: ≤20 units); PR3-ANCA was <0.2 units (normal: <0.4 (negative) units); ANA was negative (<1:160); anti-NMO antibody was negative; serum cryoglobulins were absent; anti-CCP antibody was 0.5 units/mL (normal: <5.0 units/mL); anti-beta 2 glycoprotein antibody was <9 SGU (normal: ≤20 SGU); DRVVT was negative; anticardiolipin antibodies were <9.40 (normal: 0.00–12.49 MPL); HIV was negative; RPR was non-reactive; a hepatitis panel was negative, as were a TB test and a test for Strongyloides antibodies. Cerebrospinal fluid was colorless, and demonstrated the following: The white blood cell count was 2/mm3 (normal: 0–5/mm3), and 100% of these cells were lymphocytes. The red blood cell count was 60/mm3 (normal: 0/cu mm), and all studies for infectious etiologies were negative, including EBV <2.6 log copies/mL (normal 2.6–7.6 log copies/mL), HSV, CMV PCR <2.30 log IU/mL (normal: <2.30 log IU/mL), Lyme antibody, Aspergillus antibody of <1:8 and Cryptosporidium Ag CSF.