Various drugs are known to cause musculoskeletal symptoms, such as arthralgias, myalgias, drug-induced lupus and serum sickness.1 In the rheumatology world, the most commonly recognized drugs that can cause musculoskeletal symptoms are hydralazine, minocycline, fluoroquinolones and, recently, the dipeptidyl peptidase 4 (DPP-4) inhibitor class of medications. Although beta blockers also have a noted side effect of arthralgias, as listed on the product label, there is lack of literature and awareness that this class of medications can cause arthralgias, as well as elevated anti-nuclear antibodies.2
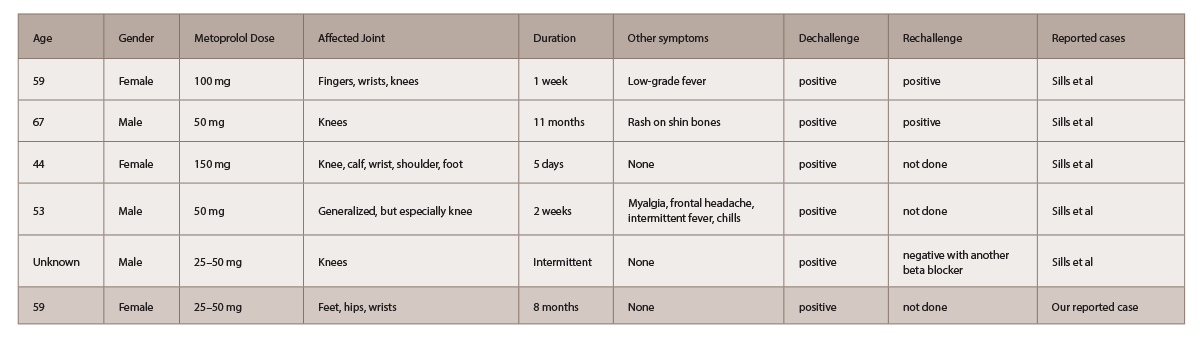
In 1986, Sills documented five cases of self-reported metoprolol-induced arthralgias through the U.S. Food and Drug Administration’s spontaneous reporting system, all of which resolved within days of discontinuing the medication (see Table 1).3 Historically, practolol caused a more severe multisystem immunologic syndrome; however, metoprolol was also found to produce a range of disease severity, from simple arthralgias to multisystem disease.4
Case Report
A 59-year-old female presented to the primary care doctor due to six to twelve months of polyarthralgias. Pain was migratory, primarily in the metatarsal joints of both feet, lateral hips and wrists. She had about 30 minutes of morning stiffness in the toes, and fingers of the right hand and low back. Pain improved with non-steroidal anti-inflammatory drugs (NSAIDs), but did not resolve.
Her prior history was significant for fluoroquinolone-induced arthralgias two years earlier after urinary tract infection treatment, as well as plantar fasciitis and trochanteric bursitis, for which she had multiple corticosteroid injections.
The patient had taken levothyroxine and sertraline for several years. She had changed from triamterene-hydrochlorothiazide to metoprolol for blood pressure control about a year earlier.
Her symptoms did not improve with exercises or NSAIDs. Following a podiatry referral, the patient went to a rheumatologist.
The examination was significant for a positive, right Finkelstein maneuver, bilateral first MTP tenderness without swelling or erythema, bilateral greater trochanteric bursa tenderness, and a positive Patrick’s maneuver bilaterally.
A prior pelvic X-ray (see Figure 1) had shown sacroiliac joint osteoarthritis and enthesopathy, which, along with the examination findings, prompted the rheumatologist to order a pelvic MRI.
Further workup, including erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), rheumatoid factory (RF), HLA B27, an ultrasound of the hand and wrist and the pelvic MRI were negative.
Metoprolol was discontinued upon the patient’s request while she was undergoing the workup, which resulted in complete resolution of her arthralgias within two to three days after drug cessation.
Discussion
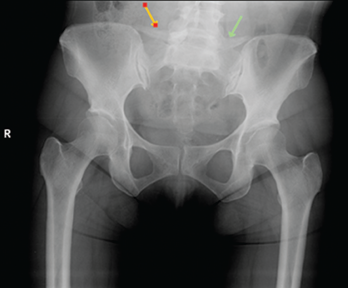
A pelvic X-ray had shown sacroiliac joint osteoarthritis and enthesopathy.
Beta blockers are increasingly prescribed medications for cardiovascular benefit and hypertension.5 Therefore, it is imperative physicians be aware of the possible side effects. From a musculoskeletal perspective, a wide array of symptoms have occurred, from arthralgias and myalgias to, less often, a systemic autoimmune phenomenon. Such an example is drug-induced lupus erythematous from practolol, a previously used beta blocker.
The pathogenesis of arthralgias is unclear at this time. In the case presented above, the patient developed symptoms of arthralgias that were out of proportion to the physical examination findings. Examination was significant only for a positive Patrick’s sign, without evidence of overt synovitis in other joints, which prompted an investigation for seronegative spondyloarthropathy. Given the subtle findings and insidious onset of symptoms, there was not substantial evidence to implicate metoprolol as the culprit.
It is likely that beta blockers are under-reported as the cause of arthralgias in patients due to lack of knowledge regarding the side effect, as well as possible confounding factors, such as electrolyte abnormalities, in patients who have these complaints.
Our patient, as well as those in the past had improvement of symptoms within days of discontinuing the medication. Thus, it is important to consider a trial off of beta blockers in a patient with arthralgias prior to pursuing further evaluation.
Saba Ziaee, MD, received her medical degree from Rush University Medical Center in Chicago. She completed a residency in internal medicine at UCLA-Olive View Medical Center and is currently completing fellowship in rheumatology at Loyola University Medical Center. Dr. Ziaee is board certified in internal medicine.
Zineb Aouhab, MD, received her medical degree from Hassan University, Medicine and Pharmacy in Casablanca, Morocco. She completed a residency in internal medicine at Stroger Hospital of Cook County and completed a fellowship in rheumatology at Northwestern Memorial Hospital. Dr. Aouhab is board certified in internal medicine and in rheumatology. She’s currently a faculty member at Loyola University Medical center.
References
- Bannwarth B. Drug-induced musculoskeletal disorders. Drug Saf. 2007;30(1):27–46.
- Boudonas GE. β-blockers in coronary artery disease management. Hippokratia. 2010 Oct;14(4):231–235.
- Sills JM, Bosco L. Arthralgia associated with beta-adrenergic blockade. JAMA. 1986 Jan 10;255(2):198–199.
- Hart FD. Drug-induced arthritis and arthralgia. Drugs. 1984 Oct;28(4):347–354.
- Youngquist S, Kaji AH, Niemann JT. Beta-blocker use and the changing epidemiology of out-of-hospital cardiac arrest rhythms. Resuscitation. 2008 Mar;76(3):376–380.