The COVID-19 pandemic has filled hospitals with patients with rapidly progressive respiratory failure and diffuse bilateral opacities on chest X-ray.1 Additionally, many patients with severe COVID-19 develop acute kidney injury and require dialysis.2 Pulmonary-renal syndromes are also important to consider in this setting. Although alveolar hemorrhage is a cardinal feature of this syndrome, many patients do not present with gross hemoptysis.3
We present a case of diffuse alveolar hemorrhage (DAH) and acute renal failure secondary to microscopic polyangiitis (MPA).
Case Description
A 38-year-old Hispanic man with past medical history of asthma presented to the emergency department in June 2020 with progressive shortness of breath over two weeks; this was accompanied by a loss of taste and smell, as well as poor appetite. He also reported associated nausea, vomiting and diarrhea. Upon presentation, he was tachypneic and in respiratory distress. He was hypoxic, with oxygen saturation 85% on 5 L/min. of oxygen by nasal cannula.
His initial laboratory results were significant for hemoglobin of 6.0 g/dL (reference range [RR]: 13.5–18.0 g/dL); hematocrit of 18.5% (RR: 40–54%); platelets 161,000/μL (RR: 150,000–450,000/μL); potassium of 7.3 mmol/L (RR: 3.5–5.1 mmol/L); bicarbonate of 11 mmol/L (RR: 24–32 mmol/L); creatinine of 30.7 mg/dL (RR: 0.7–1.3 mg/dL); blood urea nitrogen (BUN) of 153 mg/dL (RR: 9–20 mg/dL); a urinalysis showing cloudy urine with >180 red blood cells/high-powered field (hpf; RR: 0–3/hpf); proteinuria of 100 mg/dL (RR: 0–14 mg/dL);
and a white blood cell count of 14/hpf (RR: 0–4/hpf).
Arterial blood gas demonstrated a pH of 7.249 (RR: 7.35–7.45); pCO2 of 25.1 mmHg (RR: 35–45 mmHg); pO2; 63 mmHg (RR: 80–105 mmHg); and bicarbonate 11.0 mmol/L (RR: 24–32 mmol/L). Amylase and lipase were mildly elevated to 113 U/L (RR: 29–103 U/L) and 114 U/L (RR: 11–82 U/L), respectively. White blood cell count, blood glucose, aspartate transaminase (AST), alanine transaminase (ALT), bilirubin, alkaline phosphatase, lactate dehydrogenase (LDH), and troponin were all within normal limits.
A nasopharyngeal swab was performed and tested for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA, which was not detected.
A chest X-ray on admission showed bilateral airspace opacities (see Figure 1), and a chest computed tomography (CT) scan showed extensive diffuse groundglass opacities and cystic changes in both the upper and lower lobes of the lungs (see Figure 2).
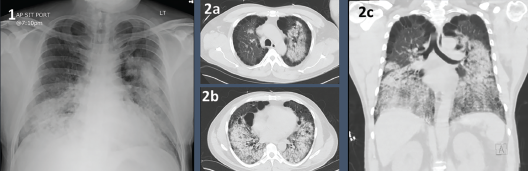
Figures 1 & 2. Figure 1: Chest X-ray with bilateral airway opacities.
Figure 2A–C: Chest CT showing extensive bilateral upper and lower lobe airway disease.


