
Figure 2a: Transverse Section
Arrowheads indicate areas of hyperlucency, suggesting air trapping, compared with hypolucent areas, indicated by arrows.
Chest radiography typically reveals clear lungs, often with hyperinflation, but HRCT of the chest is the diagnostic imaging modality of choice. Classic HRCT findings of OB-RA are mosaic attenuation and hyperinflation. Mosaic attenuation is defined as patchy areas of hyperlucency due to air trapping from bronchiolar obstruction and is best recognized during expiration (e.g., dynamic phase HRCT). Other common HRCT findings are bronchial wall thickening, cylindrical bronchiectasis and centrilobular pulmonary nodules.12
Invasive diagnostic methods are not essential to the diagnosis of OB-RA, but do help exclude alternative diagnoses. OB is characterized histologically by destruction of the bronchiolar wall by granulation tissue, effacement of the lumen, fibroproliferation and eventual replacement of the bronchiole by fibrous tissue. Lymphocytic infiltration of the bronchiolar wall has been described, but its significance is unknown. Surgical lung biopsy can provide a definite pathological diagnosis in most cases, but has significant attendant morbidity.
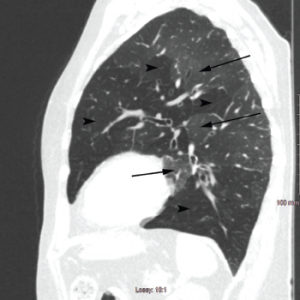
Figure 2b: Sagittal Section
Arrowheads indicate areas of hyperlucency, suggesting air trapping, compared with hypolucent areas, indicated by arrows.
Bronchoscopic methods, including transbronchial biopsies, are insensitive and are generally done to exclude other etiologies rather than make a diagnosis, as reported by Lin et al., where the diagnostic yield of transbronchial biopsy was only 28% vs. 100% for surgical biopsy.6 Similarly, Devouassoux et al. found histological pattern of constrictive bronchiolitis in eight of nine patients with OB-RA by surgical lung biopsy.7
Although the bronchoalveolar lavage (BAL) finding of neutrophilia has been reported in 10 of 12 patients with OB-RA and has been correlated with increasing disease severity in OB-transplant patients, the current level of published evidence is inadequate for definitive statements regarding diagnostic utility.
Outcome & Natural Progression: The natural progression of OB-RA is variable. The initial report of OB-RA in 1977 by Geddes et al. described a rapidly progressive disease, with five of six patients dying within 18 months.5
In contrast, Devouassoux et al. reported a mean interval of 19±32 months between symptom onset and diagnosis among 25 patients with OB-RA.7 Follow-up for more than four years showed 52% had symptomatic worsening, 32% had no change, 40% had chronic respiratory failure requiring oxygen supplementation, 4% underwent single lung transplantation, 16% died of respiratory failure, 16% had right-sided heart failure, and 100% had pulmonary hypertension on echocardiography.
Another case series that followed 32 patients for more than five years showed a 27% all-cause mortality, with an additional 15% requiring oxygen supplementation and 3% requiring lung transplantation.6

