Management: There is no standard treatment strategy for OB-RA, and despite extensive research, there is no proven treatment modality for OB-transplant.13-16 Nonetheless, growing evidence indicates early use of azithromycin in lung transplant patients may decrease the occurrence of OB, possibly via an immunomodulatory effect.17 Whether azithromycin treatment is beneficial in OB-RA is unknown.
In the absence of reliable studies, and given the putative pathogenesis of OB-RA, aggressive anti-inflammatory and biologic therapy, typically used to treat RA, is often employed in the treatment of OB-RA.
Thus, treatment of OB-RA can be divided into two categories:
- (i) Symptomatic treatment of airflow obstruction with inhaled bronchodilators: Despite the airway obstruction of OB-RA tending to be unresponsive to bronchodilators, these are recommended for symptom management; and
- (ii) Treatment of the underlying pathology and pathogenesis that focuses on RA: Options include macrolides, often with additional immunosuppressive therapy with steroids, etanercept, azathioprine or cyclophosphamide.6,18-23 Because OB is characterized by irreversible damage to the airways, it is unclear if aggressive treatment of RA can stop disease progression.
Take-Home Messages
OB is a rare pulmonary manifestation of RA, presenting as severe obstructive small-airway disease with dyspnea, bronchorrhea and cough.
The etiopathogenesis of OB-RA is not fully understood and is believed to be directly related to an autoimmune manifestation of RA.
OB-RA has a female preponderance, with mean age at diagnosis in the sixth or seventh decade. The mean interval between the diagnosis of RA and OB is around 10–15 years.
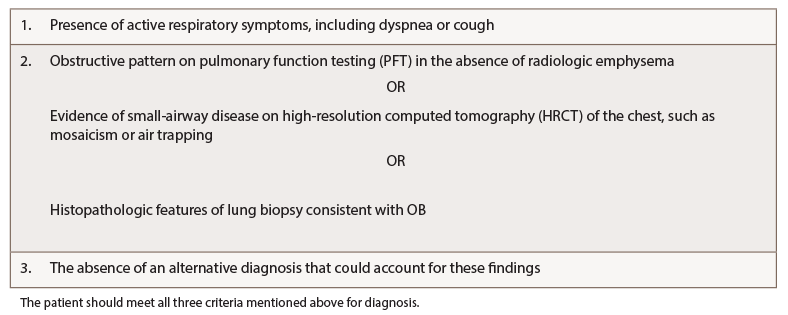
A multidisciplinary team approach, involving rheumatology, radiology and pulmonology, is essential to an accurate diagnosis and for subsequent management. Proposed diagnostic criteria include: a) the presence of active respiratory symptoms, including dyspnea or cough; b) evidence of airway obstruction noted on pulmonary function tests, imaging or histological features consistent with OB; and c) exclusion of alternative diagnosis.
PFTs classically show reduced FEV1/FVC ratio, increased residual volume and fairly preserved DLCO. HRCT is the imaging test of choice with the classic presentation of mosaic attenuation and hyperinflation. If biopsy is considered, then surgical biopsy has a better diagnostic yield compared to transbronchial biopsy.
There is no validated treatment strategy for OB-RA. Management can be divided into two broad categories: i) treatment of airway obstruction with bronchodilators and ii) treatment of underlying pathology with immunomodulator and/or immunosuppressive therapy.
 Robin Paudel, MD, is a fellow in the Pulmonary and Critical Care Department at the University of Kentucky. He did his residency in internal medicine at Jersey City Medical Center, N.J., and earned his medical degree from Manipal College of Medical Sciences, Nepal.
Robin Paudel, MD, is a fellow in the Pulmonary and Critical Care Department at the University of Kentucky. He did his residency in internal medicine at Jersey City Medical Center, N.J., and earned his medical degree from Manipal College of Medical Sciences, Nepal.