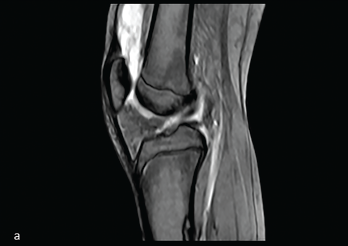
Figure 1: Midline Sagittal MRI
This image from the MRI demonstrates suprapatellar bursal fluid of mixed signal.
Intra-articular venous malformations of the knee are an uncommon cause of knee pain in children. Presenting symptoms of this rare subtype of venous malformation often include nonspecific pain and joint swelling, which may be episodic, and accompanied by limited range of motion. The signs and symptoms can mimic juvenile idiopathic arthritis (JIA).
Timely diagnosis of venous malformations is essential because lesions with intra-synovial involvement can lead to significant complications, such as joint space hemorrhage and secondary cartilage damage. Hence, improving clinical awareness of venous malformations is beneficial.
We present a rare case that illustrates the importance of prompt recognition and initiation of appropriate therapy.
Case Presentation
Our patient was a 15-year-old previously healthy female who presented to the emergency department with a four-week history of left knee pain and swelling. The patient had no history of trauma, preceding illness, fever or other joint involvement. Other systemic reviews were unremarkable.
Her left knee was warm, diffusely swollen and painful, with decreased range of motion with flexion. The rest of her joint examination was unremarkable.
Her laboratory test results, including complete blood count with differential, inflammatory markers and human leukocyte antigen B27, were unremarkable. Autoantibodies (i.e., anti-nuclear antibodies, rheumatoid factor and anti-cyclic citrullinated peptide antibodies) were absent.
Magnetic resonance imaging (MRI) of the left knee conducted at another location showed suprapatellar bursal fluid of mixed signal intensity (see Figure 1). Ultrasound of the left knee demonstrated a suprapatellar bursal effusion with complex mixed echogenicity (see Figure 2).
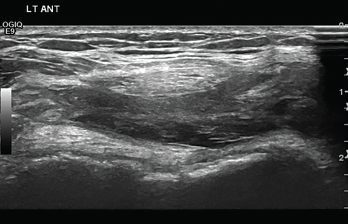
Figure 2: Transverse Ultrasound of the Anterior Knee
The ultrasound demonstrates suprapatellar bursal effusion with complex mixed echogenicity.
The patient was evaluated by an orthopedic surgeon, who recommended treatment with a scheduled non-steroidal anti-inflammatory drug and complete bed rest. However, her symptoms persisted and were worse with such activities as walking and shopping.
Therefore, she was evaluated by the rheumatology team and underwent intra-articular injection of the left knee with triamcinolone hexacetonide for presumed oligoarticular JIA.
At that time she was referred to a physical therapist.
Two weeks after the steroid injection, our patient had a significant decrease in left knee swelling and improvement in her range of motion, but the joint warmth persisted.
Four weeks later, during her physical therapy session, her left knee swelling and warmth recurred, and she had new swelling in the left ankle. Neither joint had pain or decreased range of motion.
An ultrasound of the left ankle demonstrated enlarged serpiginous vessels, and with color Doppler sampling, prominent flow within the dilated vessels was apparent (see Figure 3).

