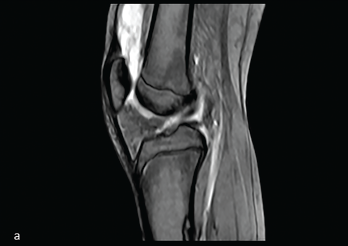
Figure 1: Midline Sagittal MRI
This image from the MRI demonstrates suprapatellar bursal fluid of mixed signal.
Intra-articular venous malformations of the knee are an uncommon cause of knee pain in children. Presenting symptoms of this rare subtype of venous malformation often include nonspecific pain and joint swelling, which may be episodic, and accompanied by limited range of motion. The signs and symptoms can mimic juvenile idiopathic arthritis (JIA).
Timely diagnosis of venous malformations is essential because lesions with intra-synovial involvement can lead to significant complications, such as joint space hemorrhage and secondary cartilage damage. Hence, improving clinical awareness of venous malformations is beneficial.
We present a rare case that illustrates the importance of prompt recognition and initiation of appropriate therapy.
Case Presentation
Our patient was a 15-year-old previously healthy female who presented to the emergency department with a four-week history of left knee pain and swelling. The patient had no history of trauma, preceding illness, fever or other joint involvement. Other systemic reviews were unremarkable.
Her left knee was warm, diffusely swollen and painful, with decreased range of motion with flexion. The rest of her joint examination was unremarkable.
Her laboratory test results, including complete blood count with differential, inflammatory markers and human leukocyte antigen B27, were unremarkable. Autoantibodies (i.e., anti-nuclear antibodies, rheumatoid factor and anti-cyclic citrullinated peptide antibodies) were absent.
Magnetic resonance imaging (MRI) of the left knee conducted at another location showed suprapatellar bursal fluid of mixed signal intensity (see Figure 1). Ultrasound of the left knee demonstrated a suprapatellar bursal effusion with complex mixed echogenicity (see Figure 2).
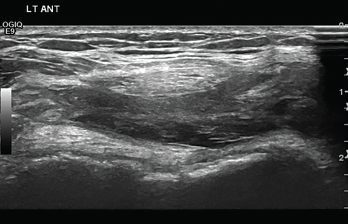
Figure 2: Transverse Ultrasound of the Anterior Knee
The ultrasound demonstrates suprapatellar bursal effusion with complex mixed echogenicity.
The patient was evaluated by an orthopedic surgeon, who recommended treatment with a scheduled non-steroidal anti-inflammatory drug and complete bed rest. However, her symptoms persisted and were worse with such activities as walking and shopping.
Therefore, she was evaluated by the rheumatology team and underwent intra-articular injection of the left knee with triamcinolone hexacetonide for presumed oligoarticular JIA.
At that time she was referred to a physical therapist.
Two weeks after the steroid injection, our patient had a significant decrease in left knee swelling and improvement in her range of motion, but the joint warmth persisted.
Four weeks later, during her physical therapy session, her left knee swelling and warmth recurred, and she had new swelling in the left ankle. Neither joint had pain or decreased range of motion.
An ultrasound of the left ankle demonstrated enlarged serpiginous vessels, and with color Doppler sampling, prominent flow within the dilated vessels was apparent (see Figure 3).
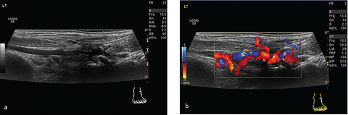
Figures 3A & 3B: Ultrasound
A) In the transverse oblique view of the anterolateral border of the left ankle, enlarged serpiginous vessels are apparent.
B) The ultrasound with overlaid color Doppler sampling demonstrates the prominent flow within the dilated vessels.
A dynamic contrast‐enhanced MRI of the lower limbs was arranged urgently, which showed early enhancement of the arteries with a prominent circumflex fibular branch arising from the anterior tibial artery and, on another view, early venous filling of the left lower leg (see Figure 4).

Figures 4A & 4B: Contrast-Enhanced MRI
A) Early enhancement of the arteries with a prominent circumflex fibular branch arising from the anterior tibial artery.
B) Early venous filling of the left lower leg.
A diagnosis of vascular malformation (venous malformation) in the left lower leg was made. She was referred to the interventional radiology clinic, where the family was counseled on the benefits and risks of an angiogram with possible embolization. The family opted for expectant management, with regular follow-up at interventional radiology and rheumatology clinics.
Discussion
Venous malformation is a congenital, low-flow, vascular malformation consisting primarily of dilated and disorganized venous channels that communicate with normal veins.1 Venous malformation of the knee is a rare but an important potential cause of unilateral knee pain in children, especially when the presentation is atypical.1,2
The clinical presentation of venous malformations in the knee, particularly pain and swelling, mimics that of juvenile idiopathic arthritis, a chronic inflammatory joint disease in children.3 Additionally, both conditions usually present at a young age and may respond favorably to non-steroidal anti-inflammatory drugs, which gives clinicians a false sense of confidence in the diagnosis.3
Venous malformation can also be mistaken for pigmented villonodular synovitis, tumors or hemangioma.
Misdiagnosis can lead to inappropriate management and treatment. Timely diagnosis of intra-articular venous malformations of the knee is essential because lesions are slowly progressive and recurrent hemarthrosis can lead to chronic synovitis and joint damage.1,2
On examination, the lesions may escape detection because they are usually situated deep within the intrafascial compartment.3 Thus, clinical history and physical examination remain essential for diagnosis. Imaging and radiological intervention play important roles in characterization and treatment.4
Cutaneous changes, such as nevus, eczema, hyper- or hypopigmentation and bluish cutaneous lesions, or prominent superficial veins can be important clinical clues; however, they present in only 29% of cases and weren’t present in our patient.1,5
Laboratory abnormalities in large venous malformations may show elevated D-dimers and hypofibrinogenemia due to continuous formation of intra-lesional microthrombi. However, these abnormalities were not seen in our patient.3,5
Our case was challenging because the initial MRI had missed the diagnosis, which could be attributed to the rarity of this disease as noted by Tsai et al.3
Importantly, one key clinical point in our case was the persistent warmth of the knee despite different treatments; this was noted by her mother and during her physical therapy sessions when she was more active.
Timely diagnosis of intra-articular venous malformations is essential because these lesions are slowly progressive & can lead to chronic synovitis & joint damage.
Treatment is based on the impact of the lesions on the patient’s quality of life, weighed against the risk of complications. In most cases, conservative treatment is recommended, but when a patient suffers clinical complications, more aggressive treatment may be considered.
Image-guided percutaneous and interventional treatments of vascular malformations are now widely accepted as first-line therapy when combined with a multidisciplinary approach to treatment. Surgical excision (i.e., synovectomy) is rarely needed.6
In Sum
Venous malformation, especially intra-articular venous malformation of the knee, can present as a clinical mimicker of juvenile idiopathic arthritis. Although the clinical presentation of these two conditions may overlap, the treatment options vary greatly. Timely diagnosis of intra-articular venous malformations is essential because lesions are slowly progressive and can lead to chronic synovitis and joint damage.
Clinical awareness of intra-articular venous malformations as an unusual cause of knee pain is important to prompt further imaging. MRI is crucial to make the diagnosis of intra-articular venous malformation of the knee and in evaluating its anatomical location and possible sequelae.1,2,4
 Eman Bamashmous, MBBS, is a fourth-year-pediatric resident at Sidra Medicine, Doha, Qatar.
Eman Bamashmous, MBBS, is a fourth-year-pediatric resident at Sidra Medicine, Doha, Qatar.
 Buthaina Al Adba, MBBS, CABP, is a pediatric rheumatologist at Sidra Medicine, Doha, Qatar.
Buthaina Al Adba, MBBS, CABP, is a pediatric rheumatologist at Sidra Medicine, Doha, Qatar.
 Sharon Bout-Tabaku, MD, MSCE, is division chief of pediatric rheumatology at Sidra Medicine, Doha, Qatar.
Sharon Bout-Tabaku, MD, MSCE, is division chief of pediatric rheumatology at Sidra Medicine, Doha, Qatar.
Acknowledgments
The authors thank Dr. Walid Mubarak and Dr. Karen Bradshaw from the Sidra Medicine radiology department for their contributions to this case.
References
- Mattila KA, Aronniemi J, Salminen P, et al. Intra-articular venous malformation of the knee in children: magnetic resonance imaging findings and significance of synovial involvement. Pediatr Radiol. 2020 Apr;50(4):509–515.
- Dalmonte P, Granata C, Fulcheri E, et al. Intra-articular venous malformations of the knee. J Pediatr Orthop. 2012 Jun;32(4):394–398.
- Tsai A, Chaudry G, Spencer S, et al. Misdiagnosis of knee venous malformation as juvenile idiopathic arthritis. J Pediatr Orthop. 2011 Sep;31(6):683–690.
- Kan JH, Hernanz-Schulman M, Damon BM, et al. MRI features of three paediatric intra-articular synovial lesions: A comparative study. Clin Radiol. 2008 Jul;63(7):805–812.
- Al-Rasheed A, Ranson M, Laxer RM. Vascular malformation as a cause of limp in a child. Arthritis Rheum. 2013 Sep;65(9):2485.
- Madani H, Farrant J, Chhaya N, et al. Peripheral limb vascular malformations: An update of appropriate imaging and treatment options of a challenging condition. Br J Radiol. 2015 Mar;88(1047):20140406.

