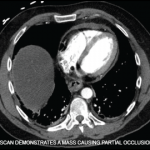
These reports and our reported case suggest that a heightened clinical index of suspicion for malignancy is warranted in patients presenting with signs and symptoms resembling AOSD. Several red flags have been reported to be associated with malignancy in AOSD, including older age, atypical rash, extremely high levels of LDH, atypical cells in the differential blood count and high levels of the soluble IL-2 receptor.13 It is unclear whether the atypical rash noted in this case report may provide diagnostic clues about the presence of an occult malignancy. Regardless, in such cases, some suggest positron emission tomography and computed tomography (PET-CT) to evaluate for the presence of solid tumors.13
Kubra Bugdayli, MD, is a board-certified rheumatologist practicing at United Hospital Center, Bridgeport, W.Va. She completed her rheumatology fellowship at UT Southwestern Medical Center, Dallas.

Dr. Eldaboush
Ahmed Eldaboush, MD, is a postdoctoral researcher at the University of Pennsylvania, Perelman School of Medicine, Philadelphia. He obtained his medical degree from Al-Azhar University, Cairo.

Dr. Aggarwal
Sanjana Aggarwal, MBBS, is a medical graduate of Hamdard Institute of Medical Sciences and Research, Delhi, India. She is currently working in a secondary level government hospital in Delhi as a junior resident in the Department of Medicine.

Dr. Bermas
Bonnie L. Bermas, MD, is the Dr. Morris Ziff Distinguished Professor in Rheumatology and clinical director of the Rheumatic Diseases Division at UT Southwestern Medical Center, Dallas.
References
- Feist E, Mitrovic S, Fautrel B. Mechanisms, biomarkers and targets for adult-onset Still’s disease. Nat Rev Rheumatol. 2018 Oct;14(10):603–618.
- Yamaguchi M, Ohta A, Tsunematsu T, et al. Preliminary criteria for classification of adult Still’s disease. J Rheumatol. 1992 Mar;19(3):424–430.
- Gerfaud-Valentin M, Jamilloux Y, Iwaz J, Sève P. Adult-onset Still’s disease. Autoimmun Rev. 2014 Jul;13(7):708–722.
- Fortna RR, Gudjonsson JE, Seidel G, et al. Persistent pruritic papules and plaques: A characteristic histopathologic presentation seen in a subset of patients with adult-onset and juvenile Still’s disease. J Cutan Pathol. 2010 Sep;37(9):932–937.
- Lee JY, Hsu CK, Liu MF, Chao SC. Evanescent and persistent pruritic eruptions of adult-onset still disease: A clinical and pathologic study of 36 patients. Semin Arthritis Rheum. 2012 Dec;42(3):317–326.
- Lee JY, Yang CC, Hsu MM. Histopathology of persistent papules and plaques in adult-onset Still’s disease. J Am Acad Dermatol. 2005 Jun;52(6):1003–1008.
- Lübbe J, Hofer M, Chavaz P, et al. Adult-onset Still’s disease with persistent plaques. Br J Dermatol. 1999 Oct;141(4):710–713.
- Ohashi M, Moriya C, Kanoh H, et al. Adult-onset Still’s disease with dermatomyositis-like eruption. J Dermatol. 2012 Nov;39(11):958–960.
- Fernández Camporro Á, Rodriguez Diaz E, Beteta Gorriti V, et al. Still disease with persistent atypical dermatomyositis-like skin eruption: Two cases associated with macrophage activation syndrome. Clin Exp Dermatol. 2022 Nov;47(11):1991–1994.
- Narváez Garcia FJ, Pascual M, López de Recalde M, et al. Adult-onset Still’s disease with atypical cutaneous manifestations. Medicine (Baltimore). 2017 Mar;96(11):e6318.
- Nagai Y, Hasegawa M, Okada E, et al. Clinical follow-up study of adult-onset Still’s disease. J Dermatol. 2012 Nov;39(11):898–901.
- Korekawa A, Nakajima K, Nakano H, Sawamura D. Paraneoplastic syndrome associated with chronic myelogenous leukemia mimicking adult-onset Still’s disease. J Dermatol. 2020 Feb;47(2):e67–e69.
- Hofheinz K, Schett G, Manger B. Adult onset Still’s disease associated with malignancy–cause or coincidence? Semin Arthritis Rheum. 2016 Apr;45(5):621–626.