
Photo 3: The patient had a purplish discoloration and digital ulcers on the distal tips of his thumb, index and middle fingers.
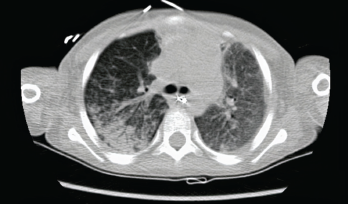
Photo 4: The initial chest CT showed diffuse bilateral airspace opacities.
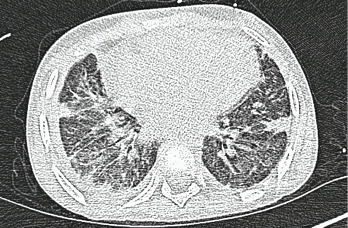
Photo 5: A high-resolution CT scan after one month shows interstitial thickening opacities and thickening of the interlobular septa.
About three weeks later, the patient presented with respiratory distress. He had been short of breath for three days, and his condition had worsened to the point that he could not complete sentences. He was taken to an emergency department for evaluation, where he was noted to be tachypneic, tachycardic and hypoxic (pulse oximeter: with ≈70% on room air), with a fever of 101ºF. The patient was placed on a non-rebreather face mask and airlifted to our pediatric intensive care unit (PICU).



