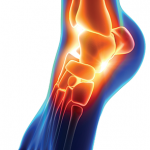
Figure 1: A lateral view of the right foot/ankle is shown with associated erythema and joint inflammation from the ankle to the forefoot. You can appreciate the associated swelling of the left medial ankle in the background, as well.
SARS-CoV-2, or COVID-19, is a complex disease entity that continues to evolve. Physicians, researchers and scientists alike have worked tirelessly to tackle this beast in its short existence; however, we are reminded daily that there is more to this virus than meets the eye. It is well known that COVID-19 can cause acute respiratory failure along with extra-pulmonary manifestations, including thromboembolic events and cardiac manifestations. Perhaps less commonly known, patients may also experience musculoskeletal manifestations.
Below, we discuss the case of a 21-year-old man who presented with inflammatory arthritis and tenosynovitis following a diagnosis of COVID-19.
Case Report
Our patient is a 21-year-old man who initially presented to the emergency department following an acute trauma, which resulted in a right sixth rib fracture. During his initial evaluation, he was mildly hypoxic and had an elevated temperature, prompting COVID-19 testing, which was found to be positive. At that time, the patient also complained of joint pain and swelling in the ankles and right wrist, presumed to be related to a sprain. He deferred admission to the hospital and was discharged home with supportive care and recommendations to treat with acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs).
The patient returned to the hospital 10 days later with persistent pain and swelling despite taking ibuprofen three times daily for the previous 10 days. The pain was debilitating, and he had been unable to bear weight for several days.
Given his symptoms, timing of development & lack of other likely causative infections, it was deemed his reactive arthritis was most likely due to COVID-19, marking yet another significant extra-pulmonary manifestation of this increasingly complex viral infection.
Upon arrival, he had a mild sinus tachycardia, but was otherwise hemodynamically stable. A physical exam revealed decreased breath sounds in the right base, with swelling in the right wrist and lower extremities with an associated erythematous rash. He had mild pain associated with active range of motion and weight bearing.
Initial laboratory findings revealed a prominent leukocytosis at 39,000 cells/μL, with profound thrombocytosis of 790,000 cells/mcL and hypoalbuminemia at 2.7 g/dL, as well. Computed tomographic imaging (CT) of the chest was notable for a right-side, potentially loculated, pleural effusion and hemothorax with adjacent hematoma.
Given the concern for sepsis, the patient was admitted to the hospital and started on broad-spectrum antibiotics. A pulmonologist was consulted to evaluate the pleural effusion. He underwent thoracentesis, which revealed an exudative effusion, although subsequent cultures were negative. The patient’s joint swelling and erythema did not improve with antibiotic treatment; therefore, a rheumatologist was consulted for further evaluation.
The patient reported that two days prior to his initial presentation to the emergency department he had developed pain, swelling and erythema in both feet and ankles, which later progressed to include the right wrist and hand, and the entire left index finger. He denied a history of joint pain and swelling. He also denied morning stiffness, urethral discharge, symptoms of inflammatory eye disease and any history of psoriasis or inflammatory bowel disease.