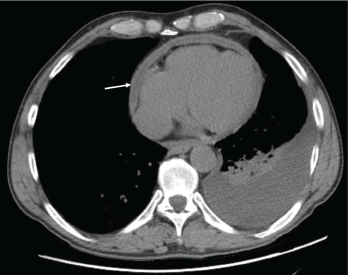
Figure 1: Pericardial effusion demonstrated on a CT of the chest. The arrow indicates the effusion.
With the input of the rheumatologist, the patient was started on rituximab infusions, and after two infusions of 1,000 mg eight weeks apart, the patient’s symptoms had resolved, his echocardiogram and inflammatory markers had normalized, and a repeat computed tomography (CT) of his chest (see Figures 1 and 2) demonstrated near-total resolution of his pericardial thickening.
The patient is currently asymptomatic and continues to receive rituximab infusions as needed (every six or 12 months) while on long-term, low-dose prednisone.
Discussion
Left untreated, RA is progressive and can lead to deterioration of cartilage and bone in the affected joints, ultimately leading to permanent disability. Involvement of extra-articular tissue occurs in approximately 40% of patients with RA and is associated with a higher mortality.1
Symptomatic pericarditis secondary to RA is uncommon, occurring in less than 10% of RA patients, but approximately 30–50% of patients have evidence of pericardial involvement on autopsy.
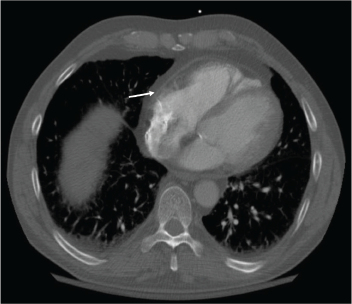
Figure 2: Resolution of the pericardial effusion was indicated on the chest CT obtained two months after initiation of rituximab infusions.
Symptomatic pericarditis secondary to RA is uncommon, occurring in less than 10% of RA patients, but approximately 30–50% of patients have evidence of pericardial involvement on autopsy.2 Episodes of tamponade and restrictive pericarditis in RA occur infrequently, and the current literature is limited to case reports.3,4 Based on current reports, surgery is the only definitive therapy known to reverse the pericardial remodeling and tamponade physiology in this patient population, and medical therapy is thought to be largely ineffective. Thus, our case presents a potentially new therapy to address a rare, but highly morbid condition.
Recent studies support a potentially effective role for rituximab in patients with active disease while on methotrexate or anti-tumor necrosis factor therapy, demonstrating that a single course of rituximab can result in clinically significant improvements in quality of life and radiographically identified disease progression within as little as 24 weeks.5 These studies were limited to patients with active articular disease, but based on our patient and his rapid recovery after initiating rituximab infusions, it is possible that anti-CD20 therapy could be a potential surgery-sparing alternative for patients with life-threatening pericardial disease.
 Scott Rodriguez, MD, is an internal medicine resident at Dartmouth-Hitchcock Medical Center, N.H.
Scott Rodriguez, MD, is an internal medicine resident at Dartmouth-Hitchcock Medical Center, N.H.
 Daniel Albert, MD, is a professor of medicine and pediatrics in the Section of Rheumatology at Dartmouth-Hitchcock Medical Center and the Geisel School of Medicine at Dartmouth. He is also a professor in the Dartmouth Institute of Health Policy and Clinical Practice. He specializes in rheumatic disease of adults and children.
Daniel Albert, MD, is a professor of medicine and pediatrics in the Section of Rheumatology at Dartmouth-Hitchcock Medical Center and the Geisel School of Medicine at Dartmouth. He is also a professor in the Dartmouth Institute of Health Policy and Clinical Practice. He specializes in rheumatic disease of adults and children.
 Kenton Powell, MD, is an internal medicine physician at Dartmouth-Hitchcock Medical Center, an assistant professor of medicine at Geisel Medical School at Dartmouth, program director of the Primary Care Track Internal Medicine Residency Program and associate program director of Categorical Track Internal Medicine Residency Program.
Kenton Powell, MD, is an internal medicine physician at Dartmouth-Hitchcock Medical Center, an assistant professor of medicine at Geisel Medical School at Dartmouth, program director of the Primary Care Track Internal Medicine Residency Program and associate program director of Categorical Track Internal Medicine Residency Program.
References
- Turesson C, O’Fallon WM, Crowson CS, et al. Occurrence of extraarticular disease manifestations is associated with excess mortality in a community based cohort of patients with rheumatoid arthritis. J Rheumatol. 2002 Jan;29(1):62–67.
- Guedes C, Bianchi-Fior P, Cormier B, et al. Cardiac manifestations of rheumatoid arthritis: A case-control transesophageal echocardiography study in 30 patients. Arthritis Rheum. 2001 Apr;45(2):129–135.
- Romanoff H, Rozin R, Zlotnick A. Cardiac tamponade in rheumatoid arthritis. A case report and review of the literature. Arthritis Rheum. 1970 Jul–Aug;13(4):426–435.
- Thould AK. Constrictive pericarditis in rheumatoid arthritis. Ann Rheum Dis. 1986 Feb;45(2):89–94.
- Cohen SB, Emery P, Greenwald MW, et al. Rituximab for rheumatoid arthritis refractory to anti-tumor necrosis factor therapy: Results of a multicenter, randomized, double‐blind, placebo‐controlled, phase III trial evaluating primary efficacy and safety at twenty‐four weeks. Arthritis Rheum. 2006 Sep;54(9):2793–2806.