Based on these symptoms, elevated disease activity score and evidence of new erosions at the level of SC joint and hands, abatacept was discontinued and rituximab was initiated. Two months later, his symptoms improved significantly and the DAS/ESR score decreased to 2.5.
It is well documented that the SC joint can be affected by traumatic or non-traumatic processes.
Discussion
The SC joint is an often neglected joint. Table 1 summarizes the pathology of the SC joint in the context of arthritides. This diarthrodial synovial joint can be affected in septic,5,14 rheumatoid,1,2,9,15 reactive,16 psoriatic11,17 and seronegative arthritis,7–9 including ankylosing spondylitis,18 gout,10 osteoarthrtitis6 or SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis and osteitis).4,19
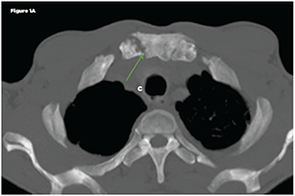
Figure 1A
Dilsen et al reported that in patients with RA, the SC joint can be affected in 40% of patients.1 Involvement of this joint can cause chest pain, tenderness to palpation, pain in the shoulder area, hypertrophy and joint crepitus on the exam.1,6,7,9 Kalliomäki et al reported that 33 of 105 patients with RA had either subchondral or marginal erosions documented by tomography, whereas chest roentgenograms were usually unremarkable.15
In our patient, the SC changes were documented at the time of chest pain evaluation. However, in the context of his active disease, new erosions were interpreted as a marker of treatment failure to abatacept, suggesting that the disease remained poorly controlled. This prompted a repeat hand X-ray, which also showed new erosions. Based on these new findings, we decided to change his treatment to rituximab, and it was noted that the patient had significant improvement in his symptoms.
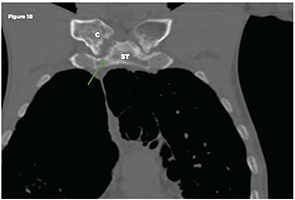
Figure 1B
Non-contrast chest CT: Axial (Figure 1A) and coronal multiplanar reformat (Figure 1B) images demonstrate bilateral sternoclavicular joint erosive arthropathy, right more than left (green arrows). A joint effusion is not identified. Key: ST-sternum, C-clavicle
The SC joint is easily accessible and can be evaluated by ultrasound, CT or magnetic resonance.1,9,15,20,21 A recent ultrasound study evaluated the SC joint in 209 RA patients and compared the findings with a group of healthy controls.20 In the RA group, 19% of scanned joints were clinically involved (meaning that patients presented with pain or swelling of the joint) compared with only 4% in the control group. Further, 43% of RA patients evaluated with ultrasound had evidence of osteophytes (29%), synovitis (15%), erosions (11%) or intra-articular power Doppler (2%), suggesting synovial hyperperfusion characteristic of an inflammatory process. When compared with the group of healthy controls, all of these findings were statistically significant. The same study reported correlation between the presence of synovitis and intra-articular power Doppler, with a higher DAS28 score.20
Conclusion
Involvement of the SC joint is not uncommon in patients with active RA. It is easily accessible for evaluation via ultrasound or CT imaging.


