
Image Credit: Kritchanut/shutterstock.com
Sternoclavicular joint involvement has rarely been reported in the context of active rheumatoid arthritis (RA).1 Traditionally, rheumatologists use serial radiographs of hands and feet to diagnose, monitor for progression or evaluate the response to treatment. The sternoclavicular (SC) joint is not a typical joint assessed for RA. However, the fact that it is a diarthrodial synovial joint suggests that this joint may be vulnerable to inflammatory process and could potentially be used radiographically to monitor disease progression.
It is well documented that the SC joint can be affected by traumatic or non-traumatic processes, such as infections (septic arthritis, osteomyelitis, tuberculosis),2–5 osteoarthritis,6 inflammatory arthritides,1,7–11 neoplasms12 and hyperparathyroidism.13
In this article, we describe a patient with long-term, poorly controlled RA who presented at our hospital with complaints of chest pain that were due to SC joint arthritis.
Case Presentation
A 52-year-old African American male with a 14-year history of seropositive (anti-CCP antibody and rheumatoid factor positive), erosive RA presented at the hospital with chest pain. He described his pain as dull, constant and located in his right upper chest, without radiation. An acute cardiovascular event was ruled out on the basis of a normal ECG and cardiac enzymes. A computerized tomogram (CT) of the chest revealed severe erosions in the right SC joint (see Figures 1A and 1B). A comparison with another chest CT obtained during the first year following his diagnosis of RA (nine years prior to this presentation) confirmed that the erosions in the SC joint were new.
The SC joint is easily accessible & can be evaluated by ultrasound, CT or magnetic resonance.
During the first five years of his RA diagnosis, the patient was treated with methotrexate, with a gradual increase in the dose up to 25 mg subcutaneous weekly. His response to treatment remained suboptimal, and the calculated disease activity score, based on a 28-joint count (DAS28/ESR), was as high as 4.5. During the subsequent three years, abatacept infusions were added (dose 750 mg monthly). Initially, the patient noted significant improvement in his symptoms, and the disease activity score improved to 2.5.
In the year prior to presentation, the patient started to complain of prolonged morning stiffness and arthralgias, and his physical exam revealed evidence of synovitis in multiple joints (i.e., bilateral metacarpophalangeal, wrists, right elbow, left knee, left ankle, bilateral metatarsophalangeal). Reassessment of his disease activity revealed a DAS28/ESR score of 5.4. X-rays of his hands documented progression of previous erosions and new erosions at the level of bilateral PIP, MCP joints and the ulnar styloid.
Based on these symptoms, elevated disease activity score and evidence of new erosions at the level of SC joint and hands, abatacept was discontinued and rituximab was initiated. Two months later, his symptoms improved significantly and the DAS/ESR score decreased to 2.5.
It is well documented that the SC joint can be affected by traumatic or non-traumatic processes.
Discussion
The SC joint is an often neglected joint. Table 1 summarizes the pathology of the SC joint in the context of arthritides. This diarthrodial synovial joint can be affected in septic,5,14 rheumatoid,1,2,9,15 reactive,16 psoriatic11,17 and seronegative arthritis,7–9 including ankylosing spondylitis,18 gout,10 osteoarthrtitis6 or SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis and osteitis).4,19
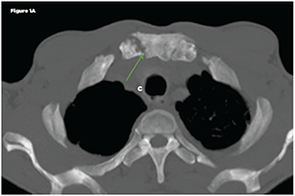
Figure 1A
Dilsen et al reported that in patients with RA, the SC joint can be affected in 40% of patients.1 Involvement of this joint can cause chest pain, tenderness to palpation, pain in the shoulder area, hypertrophy and joint crepitus on the exam.1,6,7,9 Kalliomäki et al reported that 33 of 105 patients with RA had either subchondral or marginal erosions documented by tomography, whereas chest roentgenograms were usually unremarkable.15
In our patient, the SC changes were documented at the time of chest pain evaluation. However, in the context of his active disease, new erosions were interpreted as a marker of treatment failure to abatacept, suggesting that the disease remained poorly controlled. This prompted a repeat hand X-ray, which also showed new erosions. Based on these new findings, we decided to change his treatment to rituximab, and it was noted that the patient had significant improvement in his symptoms.
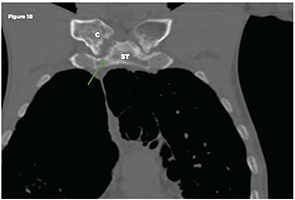
Figure 1B
Non-contrast chest CT: Axial (Figure 1A) and coronal multiplanar reformat (Figure 1B) images demonstrate bilateral sternoclavicular joint erosive arthropathy, right more than left (green arrows). A joint effusion is not identified. Key: ST-sternum, C-clavicle
The SC joint is easily accessible and can be evaluated by ultrasound, CT or magnetic resonance.1,9,15,20,21 A recent ultrasound study evaluated the SC joint in 209 RA patients and compared the findings with a group of healthy controls.20 In the RA group, 19% of scanned joints were clinically involved (meaning that patients presented with pain or swelling of the joint) compared with only 4% in the control group. Further, 43% of RA patients evaluated with ultrasound had evidence of osteophytes (29%), synovitis (15%), erosions (11%) or intra-articular power Doppler (2%), suggesting synovial hyperperfusion characteristic of an inflammatory process. When compared with the group of healthy controls, all of these findings were statistically significant. The same study reported correlation between the presence of synovitis and intra-articular power Doppler, with a higher DAS28 score.20
Conclusion
Involvement of the SC joint is not uncommon in patients with active RA. It is easily accessible for evaluation via ultrasound or CT imaging.
Diana M. Girnita, MD, PhD, is a rheumatology fellow at the University of Cincinnati, in the Department of Immunology, Allergy and Rheumatology.
Avis Ware, MD, is an associate professor of medicine at the University of Cincinnati, in the Department of Immunology, Allergy and Rheumatology. She is board certified in rheumatology and internal medicine.
Sangita Kapur, MD, is an assistant professor at the University of Cincinnati in the Department of Radiology. She is board certified in diagnostic radiology.
Christine Chhakchhuak, MD, is an assistant professor at the University of Cincinnati, in the Department of Immunology, Allergy and Rheumatology. She is board certified in rheumatology and internal medicine.
References
- Dilsen N, McEwen C, Poppel M, et al. A comparative roentgenologic study of rheumatoid arthritis and rheumatoid (ankylosing) spondylitis. Arthritis Rheum. 1962 Aug;5:341–368.
- Robinson CM, Jenkins PJ, Markham PE, et al. Disorders of the sternoclavicular joint. J Bone Joint Surg Br. 2008 Jun;90(6):685–696. doi:10.1302/0301-620X.90B6.20391.
- Saibaba B, Meena UK, Behera P, et al. Multicentric spinal tuberculosis with sternoclavicular joint involvement: A rare presentation. Case Rep Pulmonol. 2014;2014:685406. doi:10.1155/2014/685406.
- Sallés M, Olivé A, Perez-Andres R, et al. The SAPHO syndrome: A clinical and imaging study. Clin Rheumatol. 2011 Feb;30(2):245–249. doi:10.1007/s10067-010-1560-x.
- Ibrahimi A El, Daoudi A, Boujraf S, et al. Sternoclavicular septic arthritis in a previously healthy patient: A case report and review of the literature. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2009 May;13(3):e119–e121. doi:10.1016/j.ijid.2008.07.024.
- Silberberg M, Frank EL, Jarrett SR, et al. Aging and osteoarthritis of the human sternoclavicular joint. Am J Pathol. 1959 Jul–Aug;35(4):851–865.
- Jurik AG. Anterior chest wall involvement in seronegative arthritides. A study of the frequency of changes at radiography. Rheumatol Int. 1992;12(1):7–11.
- Guglielmi G, Cascavilla A, Scalzo G, et al. Imaging of sternocostoclavicular joint in spondyloarthropaties and other rheumatic conditions. Clin Exp Rheumatol. 2009 May–Jun;27(3):402–408.
- Celikyay F, Yuksekkaya R, Inanir A, et al. Multidetector computed tomography findings of the sternoclavicular joint in patients with rheumatoid arthritis. Clin Imaging. 2013 Nov–Dec;37(6):1104–1108. doi:10.1016/j.clinimag. 2013.06.006.
- Sant GR, Dias E. Primary gout affecting the sternoclavicular joint. Br Med J. 1976 Jan;1(6004):262.
- Baker H, Golding DN, Thompson M. Psoriasis and arthritis. Br Med J. 1963 Dec;2(5371):1527.
- Gehani N, Ludin A, Baskin JZ. Sternoclavicular osteoradionecrosis following treatment for head and neck cancer. Am J Otolaryngol. 2013 Nov–Dec;34(6):731–734. doi:10.1016/j.amjoto. 2013.08.012.
- Teplick JG, Eftekhari F, Haskin ME. Erosion of the sternal ends of the clavicles. A new sign of primary and secondary hyperparathyroidism. Radiology. 1974 Nov;113(2):323–326. doi:10.1148/113.2.323.
- Mozen PH, Zell SC. Sternoclavicular bacterial arthritis. West J Med. 1988 Mar;148(3):310–312.
- Kalliomäki JL, Viitanen SM, Virtama P. Radiological findings of sternoclavicular joints in rheumatoid arthritis. Acta Rheumatol Scand. 1968;14(3):233–240.
- Kumar Digge V, Meena S, Khan SA, et al. Spontaneous atraumatic dislocation of sternoclavicular joint in Reiter syndrome. Chin J Traumatol Zhonghua Chuang Shang Za Zhi Chin Med Assoc. 2012;15(4):251–253.
- Taccari E, Spadaro A, Riccieri V, et al. Sternoclavicular joint disease in psoriatic arthritis. Ann Rheum Dis. 1992 Mar;51(3):372–374.
- Good AE. The chest pain of ankylosing spondylitis. Its place in the differential diagnosis of heart pain. Ann Intern Med. 1963 Jun;58:926–937.
- Vermaat M, De Schepper AM, Bloem JL. Sternocostoclavicular hyperostosis in SAPHO-syndrome. JBR-BTR Organe Société R Belge Radiol SRBR Orgaan Van K Belg Ver Voor Radiol KBVR. 2005 May–Jun;88(3):158–159.
- Rodríguez-Henríquez P, Solano C, Peña A, et al. Sternoclavicular joint involvement in rheumatoid arthritis: Clinical and ultrasound findings of a neglected joint. Arthritis Care Res (Hoboken). 2013 Jul;65(7):1177–1182. doi:10.1002/acr.21958.
- Aslam M, Rajesh A, Entwisle J, Jeyapalan K. Pictorial review: MRI of the sternum and sternoclavicular joints. Br J Radiol. 2002;75(895):627–634. doi:10.1259/bjr.75.895. 750627.
- Sokolofff L, Gleason IO. The sternoclavicular articulation in rheumatic diseases. Am J Clin Pathol. 1954 Apr;24(4):406–414.


