A 65-year-old woman was referred by an orthopedist to a rheumatologist for left knee pain. Previously, in 2014, she underwent left total knee arthroplasty (TKA) for severe osteoarthritis in a different institution. Following the procedure, she experienced severe chronic anterolateral knee pain at rest, exacerbated by walking. Because she was rendered wheelchair bound and required chronic narcotic analgesia, she sought a second orthopedic opinion at our institution in 2015.
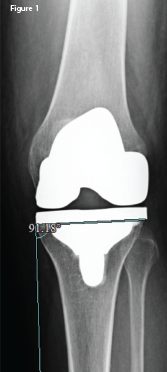
An anteroposterior X-ray of the left knee following the original arthroplasty. It shows a lateral femoral and tibial overhang of
4–5 mm and 3 mm, respectively.
An orthopedic exam revealed decreased and painful range of motion of the knee, but no lower extremity neurologic deficits. X-rays revealed significant femoral and tibial lateral overhang (see Figure 1, right) of the components. After a thorough evaluation for underlying infection, which included aspiration, bone scan and acute phase reactants, a partial revision of the left knee implant was undertaken.
The original size 4 femoral component was replaced with a size 3 component, eliminating the lateral femoral component overhang, which was found to be 4–5 mm at surgery. Following surgery, the patient’s pain improved to the point that she could walk with a cane. However, despite physical therapy, topical agents and oral non-steroidal anti-inflammatory drugs (NSAIDs), significant pain persisted, warranting further investigation.
Magnetic resonance imaging (MRI) of the lumbar spine did not reveal a radicular source of knee pain. Lower extremity venous duplex revealed no deep venous thrombosis. A trial of radiofrequency ablation of the left genicular nerves afforded only transient relief. Narcotics were still necessary, but became less effective.
The patient was then referred to a rheumatologist for evaluation of occult causes of knee pain and a sonographic evaluation to look for structural problems, such as a neuroma.
During the rheumatologic evaluation, the patient described constant, intense burning pain localized to the left lateral knee and markedly affecting activities of daily living (ADLs). Bending her knee and walking continued to intensify her pain. She denied radiation of the pain and lower extremity paresthesias.
The physical exam revealed diminished flexion of the left knee to 85º. The knee was sensitive to palpation over the anterolateral surface. Tinel’s sign over the common peroneal nerve (CPN) was negative. No evidence of left foot drop or foot dorsiflexion weakness was apparent.
The patient’s laboratory workup was entirely negative or normal including acute phase reactants, rheumatoid factor, complete blood count and comprehensive metabolic panel. X-ray revealed a 3 mm lateral overhang of the tibial component.
Ultrasound of the left knee revealed a single, deep inferior, lateral, genicular neuroma with only mild tenderness to sonopalpation. In contrast, the left CPN was markedly tender to sonopalpation. Cross-sectional areas (CSA) of the left (affected) and right (unaffected) CPNs were measured and noted to be 21 mm2 and 8 mm2, respectively (see Figure 2, below & Figure 3) Ultrasound did not demonstrate the left CPN to be hypoechoic or displaced by the protruding tibial component of the knee prosthesis.