The coexistence of ANCA-associated vasculitis with c-TMA is extremely rare. The exact prevalence and incidence are unknown, with only five case reports found in the current medical literature.4 The pathogenesis of ANCA-associated vasculitis is not fully elucidated, and the complement cascade, especially the alternative pathway, has a role in the amplification of continuing neutrophil chemotaxis and priming within the disease process. Moreover, avacopan, a C5a receptor antagonist, has demonstrated some effectiveness at inducing ANCA-associated vasculitis disease remission while limiting the use of glucocorticoids.
Typical treatment of ANCA-associated vasculitis includes glucocorticoids and either rituximab or cyclophosphamide. However, in the case of severe ANCA-associated vasculitis with a coexisting c-TMA syndrome and progressive multi-organ dysfunction, it is essential to consider the use of anti-complement therapy, such as avacopan, eculizumab and ravulizumab.
Terminal complement inhibition via eculizumab or ravulizumab, via inhibition of C5, prevents cleavage of C5 into C5a and C5b, preventing generation of the terminal complement complex C5b-9.
A theoretical advantage of inhibiting C5a, as compared with C5, is that it provides a pathway for C5b-9 to remain functional, potentially conserving some aspect of the innate immune system, especially toward encapsulated bacteria.
In the case of c-TMA, terminal complement C5b-9 would likely best be targeted due to its roles in intravascular hemolysis, as seen in other disease states, such as paroxysmal nocturnal hemoglobinuria. Additionally, the use of anti-complement therapy in c-TMA syndromes has demonstrated a lower risk of progression to end-stage renal disease.5
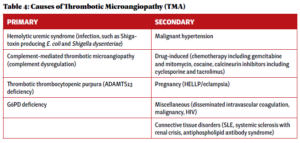
ANCA-associated vasculitis is characterized by various clinical syndromes, commonly renal and pulmonary complications. TMA syndromes in the ANCA-associated vasculitis setting are considered rare and poorly described. It is essential to evaluate for primary TMA syndromes and other systemic causes.
 Logan Oliver, MD, graduated from McGovern Medical School at UTHealth, Houston, and is currently an internal medicine resident at Naval Medical Center, San Diego.
Logan Oliver, MD, graduated from McGovern Medical School at UTHealth, Houston, and is currently an internal medicine resident at Naval Medical Center, San Diego.
 Jason J. Weiner, MD, FACP, FACR, is a rheumatologist and currently serves as chair of the Department of Medicine at Naval Medical, Center, San Diego. He completed his rheumatology fellowship at Duke University, Durham, N.C., and has research interests in health professions education.
Jason J. Weiner, MD, FACP, FACR, is a rheumatologist and currently serves as chair of the Department of Medicine at Naval Medical, Center, San Diego. He completed his rheumatology fellowship at Duke University, Durham, N.C., and has research interests in health professions education.
References
- Austin K, Janagan S, Wells M, et al. ANCA-associated vasculitis subtypes: Recent insights and future perspectives. J Inflamm Res. 2022 Apr 21;15:2567–2582.
- Fleming P, Cheung M, Sokol D. Complement-mediated thrombotic microangiopathy: A murky presentation of a rare disease entity. Blood. 2018 Nov;132(Supp 1):5005–5005.
- Kościelska-Kasprzak K, Bartoszek D, Myszka M, et al. The complement cascade and renal disease. Arch Immunol Ther Exp (Warsz). 2014 Feb;62(1):47–57.
- Shukla S, Sekar A, Naik S, et al. ANCA-associated vasculitis with systemic thrombotic microangiopathy: A review of literature. Indian J Nephrol. 2024 Mar–Apr;34(2):155–161.
- Huizenga N, Zonozi R, Rosenthal J, et al. Treatment of aggressive antineutrophil cytoplasmic antibody-associated vasculitis with eculizumab. Kidney Int Rep. 2019 Dec 4;5(4):542–545.