An extensive infectious evaluation revealed a positive plasma Mucorales polymerase chain reaction (PCR). Consequently, her treatment was switched from voriconazole to amphotericin, resulting in prompt improvement in her bone pain and normalization of her ALP levels (see Figure 4, below).
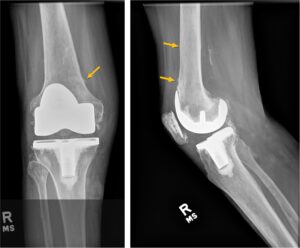
Figure 3
Right knee X-ray
Discussion
VIP is a form of skeletal fluorosis most commonly seen in patients receiving high doses and/or prolonged courses of voriconazole. Voriconazole is widely used for prophylaxis of fungal infections post-transplant and for the treatment of invasive aspergillosis.1,3,14
Excess fluoride can lead to disorganized bone formation and findings of periostitis.1 The Food and Nutrition Board at the National Academies of Sciences, Engineering, and Medicine lists the upper limit of fluoride from all sources in adults as 10 mg, based on higher levels being associated with dental and skeletal fluorosis.12 Voriconazole, a fluorinated antifungal agent, contains three fluorine atoms, compared with two in other second-generation triazole antifungal medications (e.g., fluconazole, posaconazole, isavuconazole). It has excellent oral bioavailability at 96%. It is believed that the unbound form of the drug affects bone, and 42% of the drug remains unbound by plasma proteins.3,4 Gerber et al. assessed 43 patients on triazole antifungal medication (20 of whom were taking voriconazole) and found that bone pain and radiologic evidence of periostitis were exclusively seen in patients receiving long-term voriconazole.11 This is likely because agents like posaconazole and isavuconazole, while fluorinated, do not metabolize to the free fluoride form in the body.5
A daily dose of 400 mg of voriconazole provides approximately 65 mg of fluoride, far exceeding the upper limit of safety. However, even with elevated blood fluoride levels, most individuals on voriconazole do not develop symptoms of skeletal fluorosis or periostitis, suggesting factors beyond fluoride exposure mediate VIP.
Estimates of the incidence of periostitis in those treated with voriconazole range from 15% to 50%.3,4,11 In affected individuals, periostitis and exostoses typically develop after six or more months of voriconazole therapy, although the range is variable. This variability likely reflects individual differences in past fluoride exposure, pharmacokinetics and renal clearance. The kidneys excrete 60% of daily ingested fluoride in persons with normal renal function. Higher daily and cumulative doses of voriconazole are positively correlated with the development of periostitis.3-5,11,12
Ashmeik et al. examined nine patients with VIP and 122 patients without, finding that a 31.5 g increase in cumulative voriconazole dose was associated with 8% higher odds of incident periostitis, and increased treatment duration (63 days) was associated with 7% higher odds of periostitis.15
