Discussion
Serum CK is frequently elevated in patients with hypothyroidism (57–80% cases) and in most of these cases, the associated muscle disease is mild or asymptomatic.1,2 CK levels are elevated in hypothyroidism due to direct muscle cell damage, downregulation of cellular metabolism and a reversible defect in glycogenolysis.3 However, several cases of severely high CK levels and rhabdomyolysis have been reported in the literature. Of all these cases, the mean CK level was around 16,000 U/L and the maximum CK levels reported have been around 32,000 U/L.4-7
This case is unique because the patient had hypothyroid myopathy due to low T3 from decreased peripheral conversion of T4 to T3 and inadequate T4 supplementation, in addition to underlying panhypopituitarism causing a deceptively low TSH level. Additionally, CK levels of 641,000 U/L secondary to hypothyroid myopathy leading to rhabdomyolysis has not been previously reported in medical literature, to the best of our knowledge.
This patient’s hypothyroidism is due to congenital hypopituitarism. Because of this, his TSH will not respond to T4 supplementation. On lab investigations, his T4 level was adequate, but his T3 level was not. This could have been due to lack of availability of sufficient T4 to convert to T3 peripherally.
In a typical patient, this is easy to diagnose by checking the response in TSH level to determine whether the T4 supplementation dose is adequate or not. However, this is not possible when the TSH is low because of pituitary deficiency. Theoretically, it would have been possible to give our patient larger doses of T4 supplementation to see if his T3 level improved, but it is much easier and faster to give T3 supplementation directly and assess for clinical response.
Hypothyroidism is an uncommon cause of severe rhabdomyolysis. Risk factors for precipitating rhabdomyolysis in patients with hypothyroid myopathy are vigorous exercise, coexisting hepatic or renal insufficiency and concomitant statin use.8-10 Worsening acute kidney injury or acute renal failure may occur as a secondary complication.
The diagnosis of hypothyroid myopathy is based on a thorough history and physical exam to assess for other clinical features of hypothyroidism, as well as on complete serum thyroid function testing. Clinical features of hypothyroid myopathy may include myalgias, stiffness, pseudohypertrophy (or cramps), proximal myopathy with weakness, fatigue, slowed movements and reflexes, myxedema, dry skin, hoarseness, exertional dyspnea, asymptomatic pleural or pericardial effusions, cardiomegaly and associated carpal tunnel syndrome.2,11
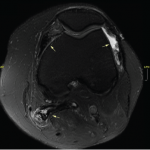
The degree of CK elevation may correlate with the severity of hypothyroidism in some but not all cases. Both electromyography and muscle biopsy findings are usually non-specific. Electromyography findings are extremely variable and can reveal abnormal, spontaneous muscle activity or, rarely, typical myopathic patterns.2,12 Muscle biopsy is usually normal or demonstrates non-specific abnormalities. Sometimes, variability in fiber size and selective atrophy of type II fibers with myofibrillar ATPase activity shift to slow fibers (type I) can occur. Sometimes, such findings as type I fiber hypertrophy, degenerating fibers, internalized nuclei and core-like structures, an increase in mitochondria distributed in perinuclear and sarcolemmal regions, and increased intracellular glycogen and lipid concentrations may occur.2,13
Treatment with thyroid hormone supplementation (T4 and/or T3 supplementation) usually leads to rapid resolution of the myopathy and rhabdomyolysis.2 Our patient will need to stay on T3 supplementation to prevent further episodes of rhabdomyolysis.