In the emergency department, a CT head scan showed subtle, low-density changes in the temporal lobes bilaterally with a lucency in the right external capsule and thalamus. A lumbar puncture (LP) followed due to initial concerns of herpes encephalitis. The LP revealed elevated protein (415.1 mg/dL) with normal glucose levels and white blood cell counts. No oligoclonal bands were present, but cerebrospinal fluid immunoglobulin G (CSF IgG) and the IgG/albumin ratio were elevated (393 mg/dL and 0.75, respectively—see Table 1). The patient was started on ceftriaxone, vancomycin and acyclovir pending culture results.
A CT chest scan revealed a large right pleural effusion. He underwent thoracentesis, and the pleural fluid analysis was exudative. A CT abdomen scan revealed mild ascites, moderate retroperitoneal edema, subcutaneous edema and external iliac adenopathy.
On day three of admission, the left-side weakness became profound, and the patient became unconscious. Brain magnetic resonance imaging (MRI) revealed an extensive abnormal signal with patchy areas of restricted diffusion, and a hyperintense T2/FLAIR signal throughout the bilateral mesial temporal lobes, extending to basal ganglia and to periventricular white matter with patchy hemorrhage concerning for acute disseminated encephalomyelitis (see Images 1–5).
Image 1A: DWI: Diffusion seen bilaterally, particularly in the mesial temporal lobe.
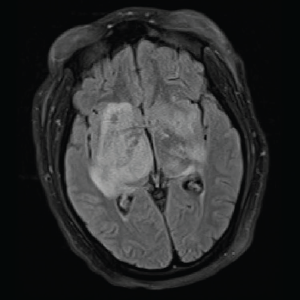
Image 1B: T2/FLAIR: Hyperintensities of the bilateral mesial temporal lobes extending into the right basal ganglia.
Image 2: DWI: Extensive abnormal signal with patchy areas of restricted diffusion, particularly in the right basal ganglia and bilateral mesial temporal lobes.
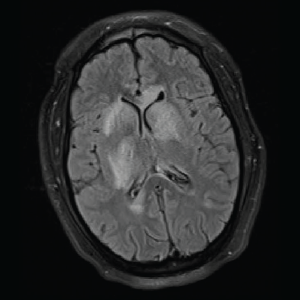
Image 3: T2/FLAIR: Hyperintensities of the caudate nucleus with mild mass effect.
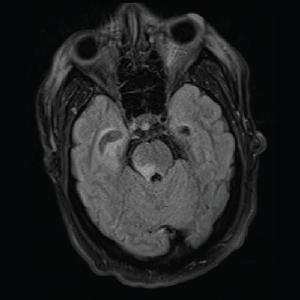
Image 4: T2/FLAIR: Abnormal T2/FLAIR signal of the right midbrain and pons.
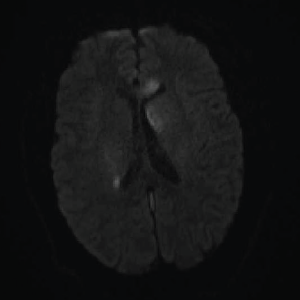
Image 5: DWI: Extensive areas of restricted diffusion extending to the periventricular white matter along the lateral ventricles.
By now a multidisciplinary team, which included infectious disease, pulmonology/critical care, rheumatology, neurology and hospitalist service, was working together to evaluate the case. They sent laboratory workup for infectious and autoimmune etiology. Complete blood count (CBC) showed normocytic anemia, lymphopenia, normal leukocytes and normal platelet counts. Inflammatory markers were elevated (ESR >130 mm/hr and C-reactive protein = 15.6 mg/dL—see Tables 1 and 2, below and opposite). A drug screen was positive for the oxycodone the patient had received a prescription for during his previous admission. Blood, urine and CSF cultures were all negative for bacterial, viral and fungal etiology (see Table 1).

