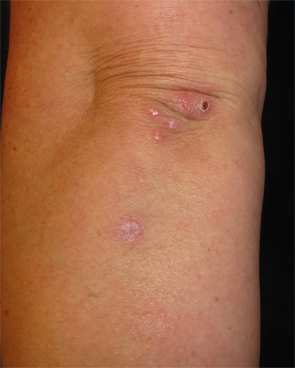
Figure 1: Erythematous, crusted papules and plaques clustered on the left elbow and extensor forearm.
The Case
A 41-year-old woman was referred to the dermatology clinic for a three-month history of tender lesions on her elbows and around the joints of her hands. Her medical history was notable for seropositive, non-erosive rheumatoid arthritis (RA), which was being treated with 5 mg prednisone daily, 10 mg methotrexate weekly by mouth, 200 mg hydroxychloroquine twice daily and 50 mg etanercept twice weekly.
She otherwise felt well and reported good control of her RA on her regimen. Her examination revealed crusted and umbilicated papules on her elbows (see Figure 1) and hands, particularly around the proximal interphalangeal and distal interphalangeal joints (see Figure 2). A chest radiograph was normal.
What’s your diagnosis?
- Rheumatoid nodules
- Psoriasis
- Palisaded neutrophilic and granulomatous dermatitis
- Perforating granuloma annulare
- Erythema elevatum diutinum
Correct Answer

Figure 2: Umbilicated and crusted papules on the volar aspects of the fingers and distal interphalangeal joints.
C. Palisaded neutrophilic and granulomatous dermatitis
Palisaded neutrophilic and granulomatous dermatitis (PNGD) is an uncommon inflammatory dermatosis characterized by discrete skin-colored to erythematous papules that appear symmetrically on the extensor aspects of the extremities with a tendency to cluster around the small joints of the hands and elbows. Lesions frequently demonstrate central umbilication and crusting. The histopathologic features of PNGD are typified by infiltrates of histiocytes forming granulomas and neutrophils that palisade around degenerated collagen fibers (see Figures 3 and 4).1 Leukocytoclastic vasculitis of the superficial dermal vasculature can be seen in early lesions.
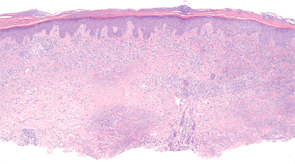
Figure 3: Histopathologic examination of palisaded neutrophilic and granulomatous dermatitis (PNGD) reveals a superficial and mid-dermal collection of histiocytes, with foci of palisading granulomas. (Hematoxylin-eosin stain; original magnification: x40.) Photomicrograph courtesy of Timothy McCalmont, MD.
The pathogenesis of PNGD is unknown, but several theories exist and include abnormal neutrophil activation, circulating immune complex deposition, a delayed-type hypersensitivity reaction, and a smoldering small vessel vasculitis.2 According to the latter hypothesis, persistent, low-grade vasculitis results in chronic tissue ischemia and collagen degeneration, which elicits a granulomatous inflammatory response. This theory is supported by the occasional observation of leukocytoclastic vasculitis in biopsies from early skin lesions.
PNGD is best considered a reactive dermatosis serving as a cutaneous marker of systemic disease as it almost invariably occurs in the setting of an underlying disorder. The most common causes are systemic lupus erythematosus and rheumatoid arthritis, followed by other autoimmune and connective tissue diseases.3 Less commonly, PNGD develops in the context of a lymphoproliferative disorder, such as acute myelogenous leukemia, multiple myeloma and non-Hodgkin lymphomas, an infection or other inflammatory conditions, such as sarcoidosis, Behçet’s disease and ulcerative colitis. Rarely, medications including the TNF-α inhibitors and chronic infections, such as hepatitis B virus and HIV infection, may precipitate PNGD.4 There is a paucity of reports of PNGD occurring in the absence of a detectable systemic disease.5,6