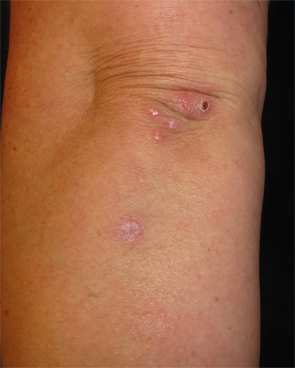
Figure 1: Erythematous, crusted papules and plaques clustered on the left elbow and extensor forearm.
The Case
A 41-year-old woman was referred to the dermatology clinic for a three-month history of tender lesions on her elbows and around the joints of her hands. Her medical history was notable for seropositive, non-erosive rheumatoid arthritis (RA), which was being treated with 5 mg prednisone daily, 10 mg methotrexate weekly by mouth, 200 mg hydroxychloroquine twice daily and 50 mg etanercept twice weekly.
She otherwise felt well and reported good control of her RA on her regimen. Her examination revealed crusted and umbilicated papules on her elbows (see Figure 1) and hands, particularly around the proximal interphalangeal and distal interphalangeal joints (see Figure 2). A chest radiograph was normal.
What’s your diagnosis?
- Rheumatoid nodules
- Psoriasis
- Palisaded neutrophilic and granulomatous dermatitis
- Perforating granuloma annulare
- Erythema elevatum diutinum
Correct Answer

Figure 2: Umbilicated and crusted papules on the volar aspects of the fingers and distal interphalangeal joints.
C. Palisaded neutrophilic and granulomatous dermatitis
Palisaded neutrophilic and granulomatous dermatitis (PNGD) is an uncommon inflammatory dermatosis characterized by discrete skin-colored to erythematous papules that appear symmetrically on the extensor aspects of the extremities with a tendency to cluster around the small joints of the hands and elbows. Lesions frequently demonstrate central umbilication and crusting. The histopathologic features of PNGD are typified by infiltrates of histiocytes forming granulomas and neutrophils that palisade around degenerated collagen fibers (see Figures 3 and 4).1 Leukocytoclastic vasculitis of the superficial dermal vasculature can be seen in early lesions.
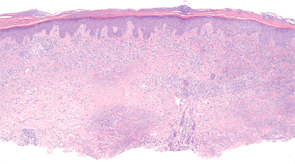
Figure 3: Histopathologic examination of palisaded neutrophilic and granulomatous dermatitis (PNGD) reveals a superficial and mid-dermal collection of histiocytes, with foci of palisading granulomas. (Hematoxylin-eosin stain; original magnification: x40.) Photomicrograph courtesy of Timothy McCalmont, MD.
The pathogenesis of PNGD is unknown, but several theories exist and include abnormal neutrophil activation, circulating immune complex deposition, a delayed-type hypersensitivity reaction, and a smoldering small vessel vasculitis.2 According to the latter hypothesis, persistent, low-grade vasculitis results in chronic tissue ischemia and collagen degeneration, which elicits a granulomatous inflammatory response. This theory is supported by the occasional observation of leukocytoclastic vasculitis in biopsies from early skin lesions.
PNGD is best considered a reactive dermatosis serving as a cutaneous marker of systemic disease as it almost invariably occurs in the setting of an underlying disorder. The most common causes are systemic lupus erythematosus and rheumatoid arthritis, followed by other autoimmune and connective tissue diseases.3 Less commonly, PNGD develops in the context of a lymphoproliferative disorder, such as acute myelogenous leukemia, multiple myeloma and non-Hodgkin lymphomas, an infection or other inflammatory conditions, such as sarcoidosis, Behçet’s disease and ulcerative colitis. Rarely, medications including the TNF-α inhibitors and chronic infections, such as hepatitis B virus and HIV infection, may precipitate PNGD.4 There is a paucity of reports of PNGD occurring in the absence of a detectable systemic disease.5,6
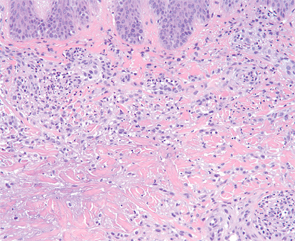
Figure 4: Higher magnification demonstrates aggregates of neutrophils and an interstitial arrangement of histiocytes. (Hematoxylin-eosin stain; original magnification: x400.) Photomicrograph courtesy of Timothy McCalmont, MD.
In patients without a preceding diagnosis of a connective tissue disorder or rheumatoid arthritis, a comprehensive evaluation is warranted and should include serologic testing for antinuclear antibodies, antineutrophil cytoplasmic antibodies (ANCAs), rheumatoid factor (RF) and cyclic citrullinated peptide, as well as a complete blood count with differential and a chest X-ray. In select cases, serum protein electrophoresis and/or immunofixation electrophoresis, viral hepatitis and HIV testing should be considered.2 Even in patients with an established systemic disease, a careful search for an underlying cause is warranted because the development of PNGD may herald the onset of an additional inflammatory or infectious process.
Because PNGD is a rare disorder, evidence for its treatment is anecdotal and limited to case reports and small series. In up to 20% of cases, PNGD resolves without intervention. Therefore, observation alone may be an acceptable management approach.2 In persistent cases, therapy should be directed toward the underlying systemic cause, as optimization of the systemic disorder often improves the skin disease. PNGD-specific treatment may be needed when a systemic association cannot be identified or when the associated condition is under control yet the skin disease persists. In such cases, dapsone, colchicine, and intralesional and systemic corticosteroids are reportedly effective.2,6
Although a benign and often self-limited condition, PNGD is an important diagnosis to recognize, because it serves as a skin sign of internal disease, particularly of autoimmune origin. Appropriate management mandates a thorough investigation to identify a precipitating cause.
Incorrect Answers
A. Rheumatoid nodules: Rheumatoid nodules are firm, semi-mobile nodules that are present in up to 20% of patients with rheumatoid arthritis, most commonly in the setting of high titers of rheumatoid factor. Similar to PNGD, these lesions often cluster around joints and on extensor surfaces including the elbows and hands (i.e., trauma-prone sites). Unlike PNGD, rheumatoid nodules can enlarge to several centimeters in size and may involve visceral organs. Accelerated rheumatoid nodulosis following initiation of methotrexate or anti-TNF-α therapy has been reported. By histopathology, rheumatoid nodules are composed of eosinophilic fibrin surrounded by a palisade of histiocytes characteristically located in the deep dermis and subcutis; unlike PNGD, neutrophils are absent. The lack of crusting, umbilication, and ulceration on clinical examination as well as the size and the distinct histopathologic features are useful to distinguish rheumatoid nodules from PNGD.
B. Psoriasis: Psoriasis is a common, chronic inflammatory skin disease typified by sharply marginated, erythematous plaques with a distinctive silver-white (“micaceous”) scale exhibiting a predilection for extensor surfaces including the elbows and knees, the scalp, presacrum and the nails. Arthritis accompanies skin disease in approximately 10–20% of cases and is more common in the setting of severe skin involvement. The location of the lesions in this case, together with overlying scale and inflammatory arthritis, may have initially suggested a psoriatic lesion, but the morphologic and histopathologic distinctions would make psoriasis unlikely. Unlike PNGD, psoriasis does not crust or umbilicate, but lesions of psoriasis may occasionally develop pustules, particularly in the acute or pustular forms of disease. The histopathologic appearance of psoriasis notably lacks a granulomatous component.
Palisaded neutrophilic & granulomatous dermatitis (PNGD) is an uncommon inflammatory dermatosis characterized by discrete skin-colored to erythematous papules that appear symmetrically on the extensor aspects of the extremities with a tendency to cluster around the small joints of the hands & elbows.
D. Perforating granuloma annulare: Granuloma annulare (GA) is an idiopathic, non-infectious granulomatous dermatitis that classically presents with small, nondescript erythematous papules that coalesce into arciform and annular plaques. Granuloma annulare often affects younger patients and develops on the hands, arms, legs and, less often, the trunk. Because of its annular configuration, GA is frequently mistaken for a superficial dermatophyte infection of the skin, but granuloma annulare’s characteristic red-brown color that accentuates with diascopy and its notable absence of scale serve as distinguishing features.
Perforating GA is an uncommon variant that displays central umbilication or focal ulceration, which corresponds to transepidermal elimination of degenerated collagen seen by histopathologic assessment. Although clinically reminiscent of PNGD, perforating GA lacks neutrophils and contains abundant mucin on histology. The overwhelming majority of cases of GA are primary or idiopathic; very rarely, atypical forms of GA have been reported in association with solid tumors and lymphomas. Whether or not a true association between generalized GA and diabetes mellitus exists is a matter of controversy.
E. Erythema elevatum diutinum: Erythema elevatum diutinum (EED) is an uncommon, small vessel vasculitis of the skin that is best regarded as a reactive neutrophilic disease. It presents with symmetrically distributed red to brown papules and plaques that favor the periarticular skin of the hands, elbows, knees and ankles. Lesions often appear non-specific and fail to develop secondary features such as crust formation or umbilication.
Although the distribution may resemble PNGD, the histopathologic features characteristically lack a granulomatous infiltrate. Instead, lesions demonstrate dense neutrophilic inflammation and almost invariably exhibit leukocytoclastic vasculitis. EED may occur in the setting of an associated disorder, most often HIV, an IgA monoclonal gammopathy, or a hematologic malignancy. It is usually not associated with an autoimmune or connective tissue disease.
Drew Kurtzman, MD, is a clinical fellow in Dermatology-Rheumatology, Department of Dermatology at Brigham and Women’s Hospital, Harvard Medical School, Boston.
Timothy McCalmont, MD, is co-director, Dermatopathology and Oral Pathology, at the University of California, San Francisco, and professor, Pathology and Dermatology, University of California, San Francisco.
Ruth Ann Vleugels, MD, MPH, is director, Autoimmune Skin Diseases Program, director, Connective Tissue Disease Clinics, program director, Dermatology-Rheumatology Fellowship Program and associate director, Education, in the Department of Dermatology, Brigham and Women’s Hospital, Boston, and assistant professor, Harvard Medical School, Boston.
Joseph F. Merola, MD, MMSc, is a dermatologist and rheumatologist, an assistant professor at Harvard Medical School, the director of clinical trials and co-director of the Center for Skin and Related Musculoskeletal Diseases at Brigham and Women’s Hospital in Boston.
References
- Chu P, Connolly MK, LeBoit PE. The histopathologic spectrum of palisaded neutrophilic and granulomatous dermatitis in patients with collagen vascular disease. Arch Dermatol. 1994 Oct;130(10):1278–1283.
- Rosenbach M, English JC 3rd. Reactive granulomatous dermatitis: A review of palisaded neutrophilic and granulomatous dermatitis, interstitial granulomatous dermatitis, interstitial granulomatous drug reaction, and a proposed reclassification. Dermatol Clin. 2015 Jul;33(3):373–387.
- Hantash BM, Chiang D, Kohler S, Fiorentino D. Palisaded neutrophilic and granulomatous dermatitis associated with limited systemic sclerosis. J Am Acad Dermatol. 2008;58(4):661–664.
- Stephenson SR, Campbell SM, Drew GS, Magro CM. Palisaded neutrophilic and granulomatous dermatitis presenting in a patient with rheumatoid arthritis on adalimumab. J Cutan Pathol. 2011 Aug;38(8):644–648.
- Misago N, Shinoda Y, Tago M, Narisawa Y. Palisaded neutrophilic granulomatous dermatitis with leukocytoclastic vasculitis in a patient without any underlying systemic disease detected to date. J Cutan Pathol. 2010 Oct;37(10):1092–1097.
- Fett N, Kovarik C, Bennett D. Palisaded neutrophilic granulomatous dermatitis without a definable underlying disorder treated with dapsone. J Am Acad Dermatol. 2011 Sep;65(3):e92–e93.