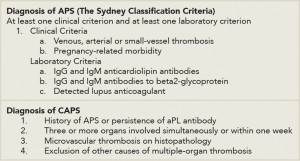
Our patient’s clinical presentation and investigations are suggestive of primary APS manifested as probable CAPS. Although he had a positive ANA, he did not meet criteria for diagnosis of systemic lupus erythematosus (SLE). CAPS is a rare and devastating condition with protean manifestations. Diagnosis is based on the presence of persistent aPL antibody positivity, multi-organ involvement within a week and microthrombosis on histopathology (see Table 4, right).1,2 Presentation depends on the organ system involved and the degree of systemic inflammatory response. As such, diagnosis is particularly challenging in the initial phases when only one organ system is involved, a patient has no prior history of APS or presents with particularly unusual manifestations, such as bleeding.
The renal, pulmonary and central nervous systems are most commonly affected. Among the pulmonary manifestations, pulmonary embolism is most prevalent, but there have been reported cases of pulmonary hemorrhage.
Most cases of CAPS are associated with a precipitant, such as infection, surgery, subtherapeutic anticoagulation or SLE flares.1 More than one in three patients with CAPS will die. Thus, preventing CAPS and the aggressive treatment of cases are imperative.1
Anticoagulation with unfractionated or low molecular weight heparin for at least one week, followed by oral anticoagulants, is the mainstay of treatment.1 High-dose glucocorticosteroids are also used as a first-line intervention to contain the inflammatory response associated with CAPS. Treatment should continue for at least three days. In addition to steroids, plasmapheresis is used to curtail the inflammatory response by removing the antiphospholipid antibodies and inflammatory mediators. Likewise, intravenous immunoglobulin is also potentially useful, but it should be used with caution in patients who are concurrently bleeding because anticoagulants cannot be used to ameliorate its potentially prothrombotic effect. Other treatments include cyclophosphamide, which is found to be most useful in SLE-associated CAPS, and rituximab and eculizumab have also been used in limited cases.1,3
In the rare circumstance that a patient presents with bleeding, then immediate management should be targeted at ensuring a secure airway, maintaining oxygenation and ventilation and preventing circulatory collapse by adequate resuscitation using intravenous fluids and blood products as necessary. In addition to adequate resuscitation, attempts should be made to arrest bleeding by local control at the source and correcting coagulopathy. Of note, a prolonged aPTT in APS and CAPS is an in vitro manifestation of the lupus anticoagulant and indicates a tendency toward a procoagulant state. Therefore, utilizing the aPTT as the sole indication of a coagulopathy that needs correction is not useful in these patients. Instead, the complete picture inclusive of other coagulation studies should be taken into consideration. These include assessment of the PT/INR, thrombin time, factor assays, appropriate mixing studies, platelet count and platelet function tests, fibrinogen and fibrin degradation product levels and thromboelastography, where clinically appropriate.